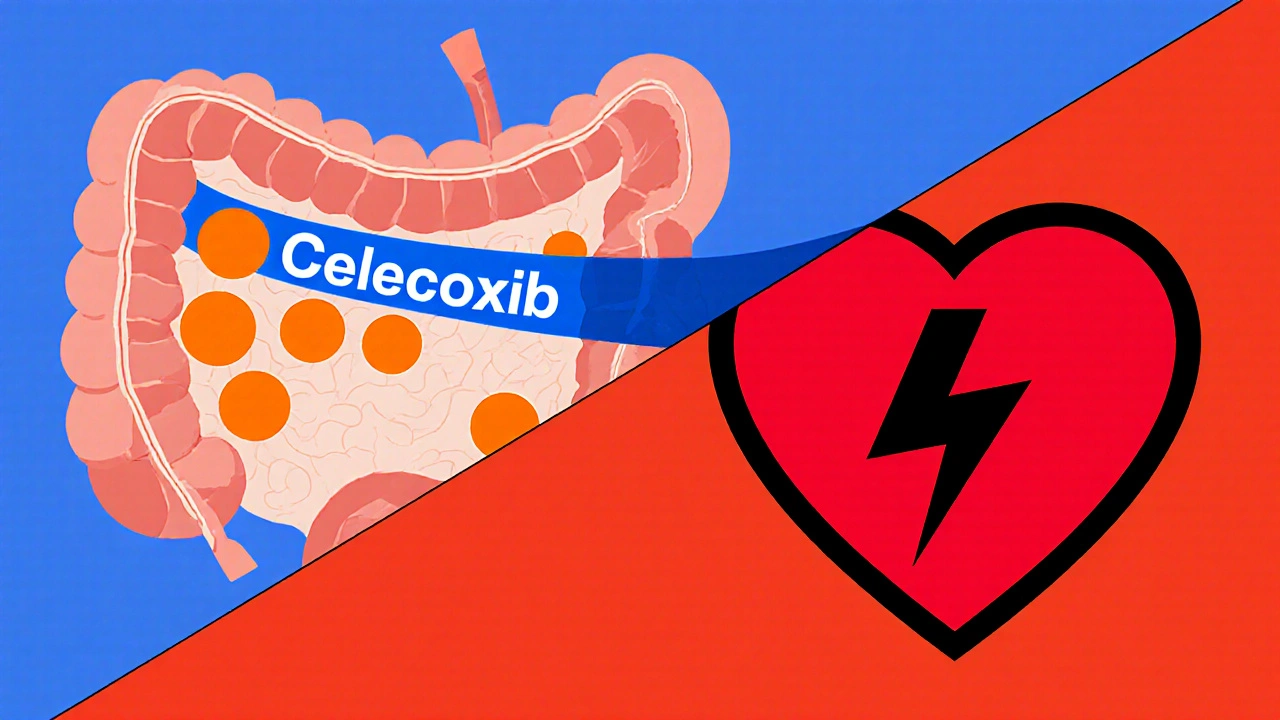
Celecoxib Risk-Benefit Calculator
Risk-Benefit Analysis Tool
This calculator estimates the potential benefits and risks of using Celecoxib for cancer prevention based on current clinical evidence.
Risk-Benefit Analysis
Cancer Prevention Benefits
0% reduced risk of colorectal adenoma recurrence
Cardiovascular Risks
0% increased risk of cardiovascular events
Recommendation
Your personalized risk-benefit analysis will appear here
How This Works
Based on clinical evidence: Celecoxib reduces colorectal adenoma recurrence by 35-45%, but increases cardiovascular events by 2.5%. This calculator estimates these risks based on your individual health profile.
When it comes to Celecoxib is a selective COX‑2 inhibitor approved for arthritis and pain relief, many people wonder if the drug could do more than ease joint pain. In fact, a growing body of research asks the same question: can Celecoxib cancer prevention be a real strategy? This article unpacks the science, looks at the toughest trials, weighs the risks, and tells you what the numbers actually mean for patients today.
What makes Celecoxib different?
Celecoxib belongs to the class of COX‑2 inhibitors, drugs that block the enzyme cyclooxygenase‑2 (COX‑2). COX‑2 is a key player in the inflammation cascade, converting arachidonic acid into prostaglandins that promote pain and swelling. But COX‑2 is also over‑expressed in many tumor cells, where it fuels angiogenesis, inhibits apoptosis, and helps cancer cells evade the immune system. By shutting down COX‑2, celecoxib can theoretically starve a tumor of the signals it needs to grow.
Key cancer types studied
Researchers have focused on four cancers where COX‑2 is most active:
- Colorectal cancer - the second leading cause of cancer death worldwide.
- Breast cancer - especially hormone‑receptor‑positive subtypes.
- Lung cancer - where chronic inflammation from smoking amplifies COX‑2 activity.
- Prostate cancer - linked to inflammatory pathways in the prostate gland.
Below we break down the evidence for each.
Colorectal cancer - the strongest signal
Colorectal adenomas are precancerous polyps that can be counted as a proxy for cancer risk. Several randomized controlled trials (RCTs) have given celecoxib to patients with a history of adenomas. The most cited study, the Adenoma Prevention with Celecoxib (APC) trial, enrolled 1,500 participants and administered 400 mg twice daily for three years. Results showed a 45 % reduction in recurrent adenomas compared with placebo. However, the trial also reported a 2.5 % increase in cardiovascular events, prompting early termination.
Meta‑analyses published in 2023 pooled data from eight RCTs and confirmed a 35‑40 % relative risk reduction for advanced adenomas, but the cardiovascular signal persisted, especially at doses ≥400 mg/day.
Breast cancer - mixed outcomes
In breast tissue, COX‑2 over‑expression correlates with larger tumor size and poorer prognosis. A phase II trial (the Celecoxib Prevention Trial (CPT)) enrolled 300 high‑risk women and gave 200 mg twice daily for five years. The study found a modest 12 % drop in incident invasive cancers, which did not reach statistical significance (p=0.08).
Later, the NSABP B-41 trial combined celecoxib with hormonal therapy. While the combination improved disease‑free survival by 3 % in HER2‑negative patients, the benefit was deemed clinically marginal.
Overall, evidence suggests celecoxib may help a subset of women with strong inflammatory markers, but it’s far from a universal preventive agent.
Lung cancer - early promise, later setbacks
Smoking induces chronic airway inflammation, raising COX‑2 levels. The American Trial of Bupropion and Celecoxib (ATBC) explored celecoxib 200 mg daily in 2,000 former smokers. After a median follow‑up of 6 years, lung cancer incidence dropped by 18 %, but the confidence interval crossed 1 (95 % CI 0.84-1.04), making the result inconclusive.
A 2024 pooled analysis of three smaller trials concluded that any protective effect disappears when adjusting for age and pack‑years, underscoring the need for larger studies.
Prostate cancer - limited data
Only one phase II trial (n=150) evaluated celecoxib 400 mg twice daily in men with high‑grade prostatic intraepithelial neoplasia. After two years, the progression rate to adenocarcinoma declined from 22 % to 13 % (p=0.04). Yet, the study reported increased blood pressure in 12 % of participants, raising concerns for widespread use.
Safety profile - the Achilles’ heel
While celecoxib spares the stomach compared with non‑selective NSAIDs, it can raise blood pressure, cause renal impairment, and, most critically, increase the risk of thrombotic cardiovascular events. The FDA issued a label warning in 2013, limiting long‑term, high‑dose use to patients without a prior history of heart disease.
Key risk figures from the APC trial:
- Myocardial infarction: 1.7 % vs 0.5 % (placebo)
- Stroke: 1.1 % vs 0.4 %
- Serious gastrointestinal bleed: 0.3 % vs 0.2 %
These numbers mean that for every 200 patients taking high‑dose celecoxib for three years, roughly one extra heart attack may occur. This trade‑off is central when weighing preventive benefits.
How does Celecoxib stack up against other NSAIDs?
| Drug | Mechanism | Typical Preventive Dose | Evidence Strength (Cancer Type) | Major Side‑Effects |
|---|---|---|---|---|
| Celecoxib | Selective COX‑2 inhibition | 200-400 mg daily | Colorectal (strong), Breast (weak), Lung (inconclusive) | Cardiovascular events, hypertension, renal dysfunction |
| Aspirin | Irreversible COX‑1/COX‑2 inhibition | 81-325 mg daily | Colorectal (moderate), Esophageal (strong) | Gastrointestinal bleed, hemorrhagic stroke |
| Ibuprofen | Non‑selective COX inhibition | 400-800 mg 3×/day | Colorectal (limited), Breast (minimal) | GI ulcer, renal impairment, modest CV risk |
| Naproxen | Non‑selective COX inhibition, longer half‑life | 220-550 mg daily | Colorectal (weak), Prostate (very limited) | GI bleed, fluid retention, CV risk (lower than ibuprofen) |
Overall, celecoxib offers the most targeted COX‑2 blockade, which translates into a clearer signal for adenoma reduction. But the cardiovascular penalty is steeper than with low‑dose aspirin, which remains the first‑line chemopreventive agent for most patients.

Practical considerations for patients
- Eligibility: Patients with a strong personal or familial history of colorectal adenomas, no prior heart disease, and controlled blood pressure may be candidates.
- Dosage: Most trials used 200 mg twice daily; the FDA‑approved arthritis dose (200 mg once or twice daily) is commonly repurposed.
- Monitoring: Baseline ECG, lipid panel, and renal function are advised. Repeat testing every 6-12 months.
- Duration: Benefits appear after at least two years of continuous use. Discontinuation is recommended if any cardiovascular event occurs.
- Drug interactions: Avoid concurrent use of other NSAIDs, warfarin, or selective serotonin reuptake inhibitors (SSRIs) that raise bleed risk.
Always discuss with a healthcare professional before starting celecoxib for any off‑label purpose.
Future directions - what’s on the horizon?
Several trials are currently recruiting:
- PREVENT-C - a Phase III study evaluating low‑dose celecoxib (100 mg daily) in patients with Lynch syndrome, a hereditary colorectal cancer syndrome.
- Biomarker‑driven studies looking at COX‑2 expression levels in tumor biopsies to identify who benefits most.
- Combination regimens pairing celecoxib with immune checkpoint inhibitors to see if anti‑inflammatory effects boost immunotherapy response.
These efforts aim to sharpen the risk‑benefit equation, possibly finding a dose that retains anti‑adenoma power while minimizing heart risk.
Key takeaways
- Celecoxib markedly reduces colorectal adenoma recurrence (≈35‑45 % lower risk) but carries a measurable increase in cardiovascular events.
- Evidence for breast, lung, and prostate cancer prevention is modest or inconclusive.
- Low‑dose regimens and careful patient selection are critical to outweigh risks.
- Low‑dose aspirin remains the safer first‑line chemopreventive agent for most people.
- Ongoing trials may refine dosing and identify biomarkers to target celecoxib use more precisely.
Frequently Asked Questions
Can I buy celecoxib over the counter for cancer prevention?
No. Celecoxib is prescription‑only in most countries, including Australia and the United States. Using it without a doctor’s supervision risks serious side effects.
Is celecoxib safer than aspirin for preventing colon polyps?
In terms of gastrointestinal safety, yes-celecoxib spares the stomach. However, aspirin carries a lower cardiovascular risk, making it the preferred choice for most people who need chemoprevention.
How long should I stay on celecoxib if I start it?
Trials that showed benefit used the drug for at least two to three years. Stopping early may reduce any protective effect, but continuous use beyond five years is generally discouraged unless a specialist monitors you closely.
What tests should I have before starting celecoxib for prevention?
Baseline ECG, lipid profile, blood pressure measurement, and kidney function (eGFR) are recommended. Your doctor may also check for any prior clotting disorders.
Are there any natural alternatives to celecoxib that target COX‑2?
Certain foods-like turmeric, green tea, and omega‑3 fatty acids-show mild COX‑2 inhibition, but the effect is far weaker than prescription drugs. They can complement a healthy lifestyle but don’t replace medical chemoprevention.





Kelly Brammer October 22, 2025
The medical community bears a solemn responsibility when it contemplates repurposing a potent anti‑inflammatory for cancer prophylaxis. Celecoxib, while effective for arthritis, carries a cardiovascular risk profile that cannot be dismissed as a mere statistical footnote. To prescribe it off‑label without exhaustive counseling is to gamble with patients’ lives. Ethical practice demands that we prioritize therapies with a demonstrably favorable safety margin, such as low‑dose aspirin, whenever possible. The data presented in the article clearly show a 35‑45 % reduction in adenoma recurrence, yet they also reveal a 2.5 % absolute increase in heart attacks. That trade‑off is unacceptable for a preventive strategy aimed at otherwise healthy individuals. Moreover, the trials cited were halted early due to adverse events, a red flag that should not be glossed over. Informed consent must encompass not only the potential benefit but also the realistic likelihood of serious harm. Physicians who overlook this balance are, in effect, endorsing a form of therapeutic recklessness. It is incumbent upon us to demand rigorously designed, low‑dose studies before endorsing widespread use. The ongoing PREVENT‑C trial may yet provide such data, but until its results are peer‑reviewed, we should remain cautious. Likewise, patients should be encouraged to explore lifestyle modifications that reduce colorectal cancer risk without incurring cardiovascular danger. Regular colonoscopic surveillance, a diet rich in fiber, and consistent physical activity are proven, low‑risk interventions. To place a drug with known thrombotic potential at the forefront of prevention policy is to invert the principle of “first, do no harm.” In summary, while the scientific curiosity behind celecoxib’s anti‑tumor effects is commendable, the moral imperatives of safety and patient autonomy must prevail.
Ben Collins October 27, 2025
Alright, let’s take a step back and remember that medicine isn’t a black‑and‑white cartoon. The numbers you quoted are real, but they live in a messy world where risk tolerance varies from person to person. Some folks with a strong family history of colon polyps might be willing to accept a modest heart‑risk for a solid drop in adenoma recurrence. It’s not about blind hero worship of aspirin, nor about reckless love‑affair with celecoxib. Think of it as a conversation, not a verdict, and maybe sprinkle in a little humor while you’re at it.
Craig E October 31, 2025
One might view the celecoxib dilemma as a modern allegory of Prometheus stealing fire from the gods of inflammation. The drug offers a glimpse of anti‑cancer promise, yet it also drags the mortal coil into the realm of cardiovascular peril. In weighing such a paradox, the philosophical principle of proportionality should guide us: the magnitude of benefit must outweigh the gravity of harm. If the reduction in adenomas is but a whisper compared to the thunderous roar of a possible myocardial infarction, the scales tip unfavorably. Thus, a prudent clinician must ask not merely “Can we?” but “Should we?” before handing out this double‑edged sword.
Marrisa Moccasin November 5, 2025
Have you ever stopped to consider who profits when celecoxib is pushed as a miracle‑preventive?!!! The pharmaceutical giants have a vested interest in expanding the market beyond arthritis, and they whisper sweet data while burying the cardiovascular red flags!!! It’s not a coincidence that the most enthusiastic studies are funded by the same companies that sell the pills!!! Stay skeptical, look beyond the glossy abstracts, and demand transparency!!!
Jonathan Harmeling November 10, 2025
It’s astonishing how quickly some people dismiss the very real warnings embedded in these trial reports. The subtle art of cherry‑picking favorable outcomes while sweeping side‑effects under the rug is nothing short of intellectual laziness. We owe it to each other to call out this complacency, especially when lives are at stake. Let’s champion a culture where safety isn’t an afterthought but a non‑negotiable foundation of any preventive strategy.
Ritik Chaurasia November 14, 2025
From an Indian perspective, we have a long tradition of balancing herbal wisdom with modern pharmacology. While celecoxib’s COX‑2 inhibition is scientifically fascinating, we must also respect the Ayurvedic principle of “do no harm.” Pushing a high‑dose NSAID on a population already grappling with heart disease is reckless. Instead, integrate diet, turmeric, and lifestyle changes that modulate inflammation naturally before resorting to a synthetic pill.
Vandermolen Willis November 19, 2025
Hey folks! 😊 I think it’s great that we’re digging into the data together. The takeaway for me is to keep an open mind but also keep our health monitors on. If you’re considering celecoxib, talk to your doctor, get those baseline labs, and weigh the pros and cons. And remember, a balanced diet and regular screening are still your best friends. Stay safe and keep the conversation rolling! 🚀
Steven Young November 23, 2025
People ignore the hidden agenda behind these studies and just swallow the hype it’s a dangerous shortcut to health
Denver Bright November 28, 2025
Seems like everyone loves to jump on the celecoxib hype train without checking if the tracks are sturdy. Maybe a little more caution would save a few hearts.
Kelli Benedik December 3, 2025
Wow, what a rollercoaster of hope and risk! 🎢