Most people with chronic kidney disease (CKD) don’t know they have it. Not because they’re ignoring symptoms, but because there are no symptoms-at least not until the damage is serious. By the time fatigue, swelling, or nausea show up, the kidneys have already lost half their function. That’s why early detection isn’t just helpful-it’s the only thing that can stop CKD from becoming kidney failure.
What Chronic Kidney Disease Really Means
Chronic kidney disease isn’t a single illness. It’s a label for any lasting damage to the kidneys that affects how they filter waste and fluid from your blood. This damage lasts longer than three months. It doesn’t always mean your kidneys are failing. In fact, most people with CKD are in the early stages, where the kidneys still work-but they’re working harder than they should.
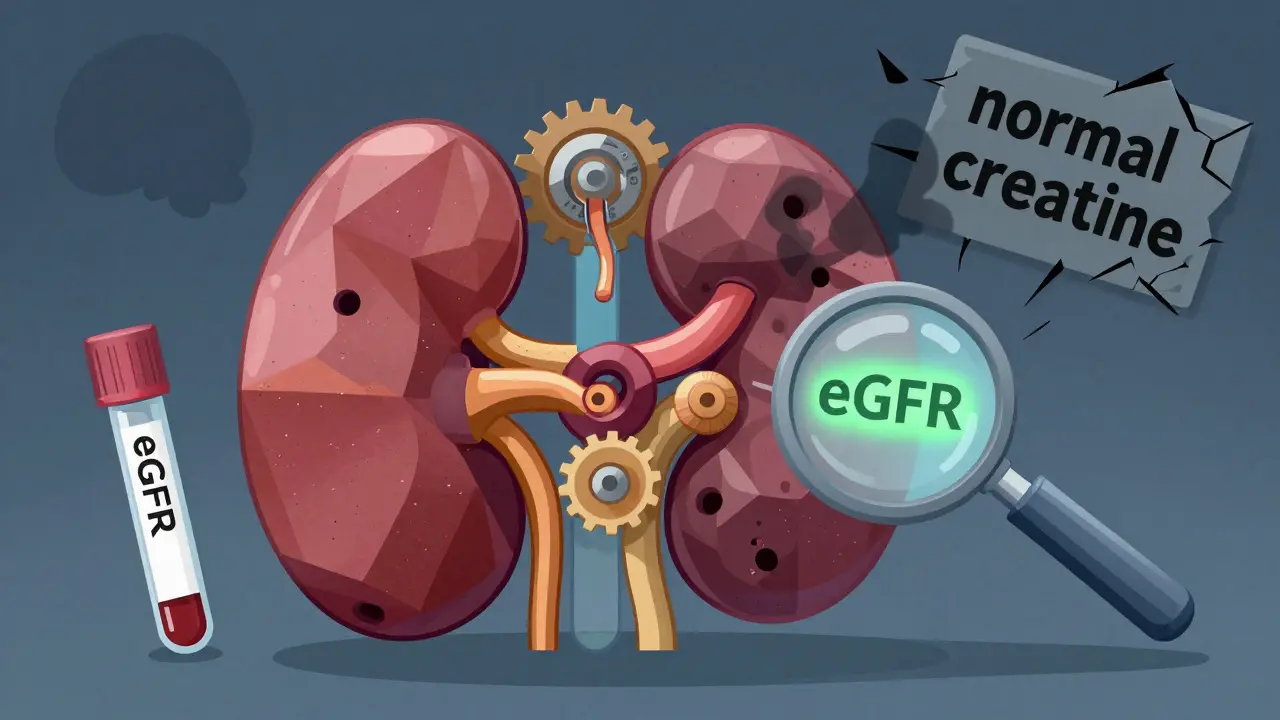
The old way of diagnosing CKD was simple: check your creatinine level, calculate your eGFR, and call it a day. But that missed up to 40% of cases. Why? Because creatinine levels vary wildly based on muscle mass, age, diet, and even race. A healthy 80-year-old with low muscle mass might have a normal creatinine but still be losing kidney function. A young, muscular person might have high creatinine but perfectly healthy kidneys. Relying on one number was like trying to judge a car’s condition by checking the fuel gauge alone.
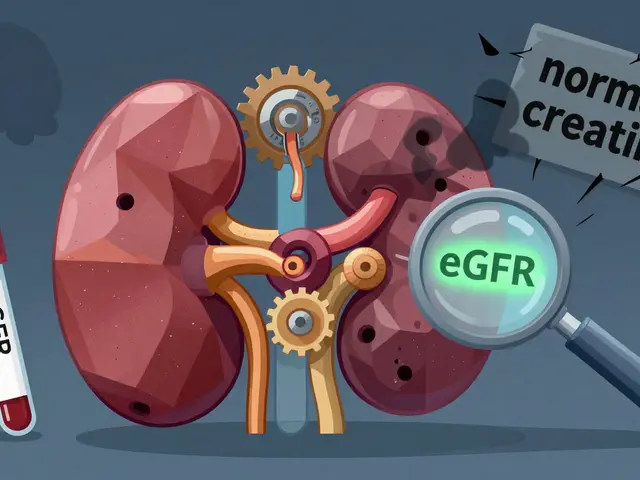
Today, the standard is two tests: eGFR and uACR. You need both. Neither one alone is enough.
The Two Tests That Catch CKD Early
eGFR (estimated glomerular filtration rate) tells you how well your kidneys are filtering. It’s calculated using your blood creatinine level, age, sex, and race. The current gold standard is the CKD-EPI equation, updated in 2009 to be more accurate than older formulas. But even this has limits. That’s why we need the second test.
uACR (urine albumin-to-creatinine ratio) measures how much protein-specifically albumin-is leaking into your urine. Healthy kidneys keep protein in the blood. When they’re damaged, even tiny amounts of albumin slip through. A uACR of 30 mg/g or higher means kidney damage is happening, even if your eGFR is still normal.
This two-test rule is the foundation of modern CKD diagnosis. The KDOQI and KDIGO guidelines made it official in 2012. Before that, many people were told they were fine because their creatinine looked okay. Now we know: if your uACR is high, your kidneys are under stress-even if your eGFR is 80 or 90.
For people with diabetes or high blood pressure, these tests should be done every year. If you’re over 60, have a family history of kidney disease, or are African American, Native American, or Hispanic, you’re at higher risk. That means you need screening, not waiting.
CKD Stages: Knowing Where You Stand
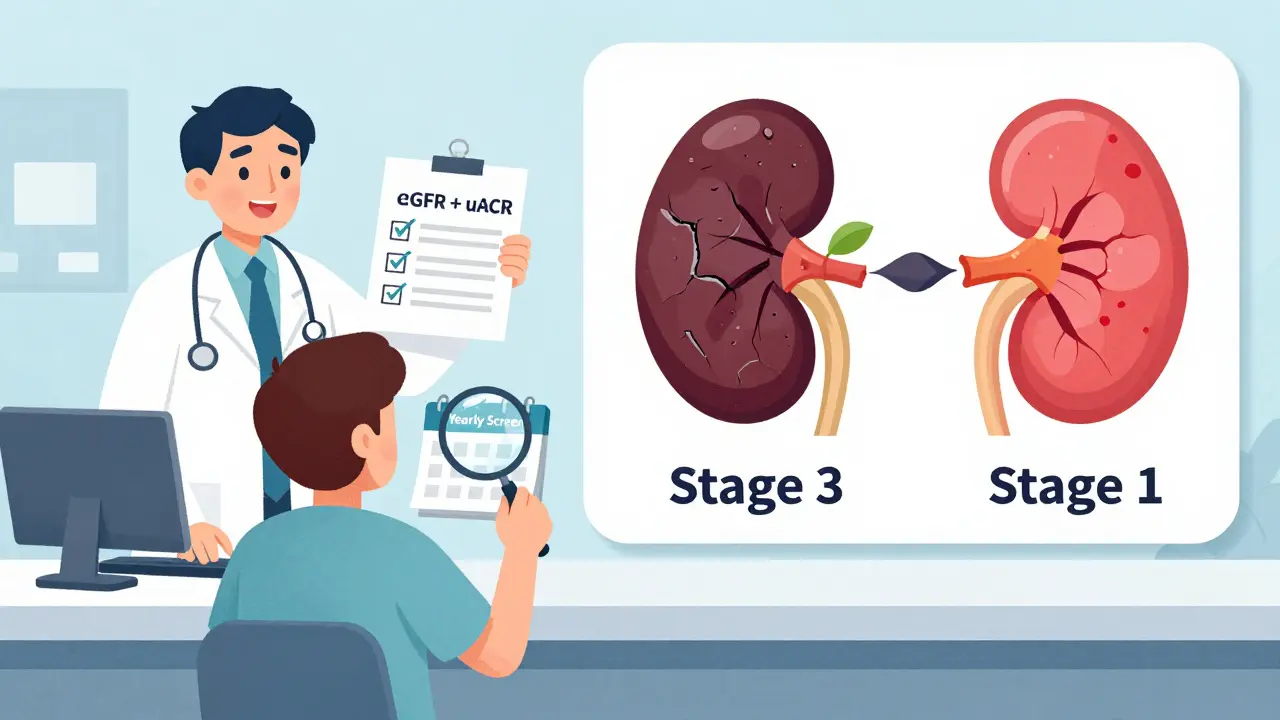
CKD is divided into five stages, based on eGFR and whether there’s kidney damage. But here’s the key: stages 1 and 2 are where you still have time.
- Stage 1: eGFR ≥90, but uACR ≥30 mg/g. Kidneys are working fine, but damage is present.
- Stage 2: eGFR 60-89, uACR ≥30 mg/g. Slight loss of function, but still plenty of reserve.
- Stage 3a: eGFR 45-59. Moderate decline. This is where many people first get diagnosed.
- Stage 3b: eGFR 30-44. More serious loss. Risk of complications rises.
- Stage 4: eGFR 15-29. Severe damage. Planning for dialysis or transplant often begins here.
- Stage 5: eGFR <15. Kidney failure. Dialysis or transplant needed.
Here’s what matters: if you’re in stage 1 or 2, you can stop progression. If you’re in stage 4 or 5, you’re managing decline. The window to act is wide open in the early stages-and it closes fast.
How to Stop CKD From Getting Worse
Early detection only helps if you do something about it. And the good news? Simple steps make a huge difference.
Control your blood pressure. Keeping it under 130/80 mmHg (not 140/90) cuts the risk of kidney damage worsening by 27%. That’s from the SPRINT trial. Medications like ACE inhibitors or ARBs are often used-they don’t just lower blood pressure, they protect the kidneys.
Manage your blood sugar. If you have diabetes, your kidneys are under constant stress. Tight glucose control slows damage. SGLT2 inhibitors (like dapagliflozin and empagliflozin) were originally diabetes drugs-but now they’re used for CKD too. The CREDENCE trial showed they reduce progression to kidney failure by 32% in people with albuminuria.
Watch what you eat. Too much salt? It raises blood pressure. Too much protein? It can strain damaged kidneys. A diet low in sodium, moderate in protein, and rich in fruits and vegetables helps. You don’t need a fancy plan. Just cut processed foods, avoid canned soups, and skip the salt shaker.
Avoid NSAIDs. Ibuprofen, naproxen, even aspirin in high doses can harm kidneys, especially if you already have CKD. Use acetaminophen instead for pain. Always check with your doctor before taking any new medication.
Stop smoking. Smoking narrows blood vessels, including those in the kidneys. It speeds up damage. Quitting is one of the most effective things you can do.
Why Most People Still Miss It
Even with clear guidelines, CKD is still underdiagnosed. A 2022 study found only 52.7% of primary care doctors consistently order both eGFR and uACR. In rural clinics, that number drops to 31.7%. Why?
- Electronic health records don’t remind doctors to order both tests.
- Some think “normal creatinine” means “no problem.”
- Urine tests feel like an extra step. But a simple dipstick or spot sample is all it takes.
Patients aren’t blameless, either. Many don’t know they’re at risk. One Reddit user shared: “My doctor only checked creatinine for 10 years despite my diabetes. By the time they did uACR, I was stage 3.” That’s not rare.
But there’s hope. The National Kidney Foundation found that when patients get visual charts showing their CKD stage (not just numbers), they’re 28% more likely to follow their treatment plan. Seeing the damage helps people take it seriously.
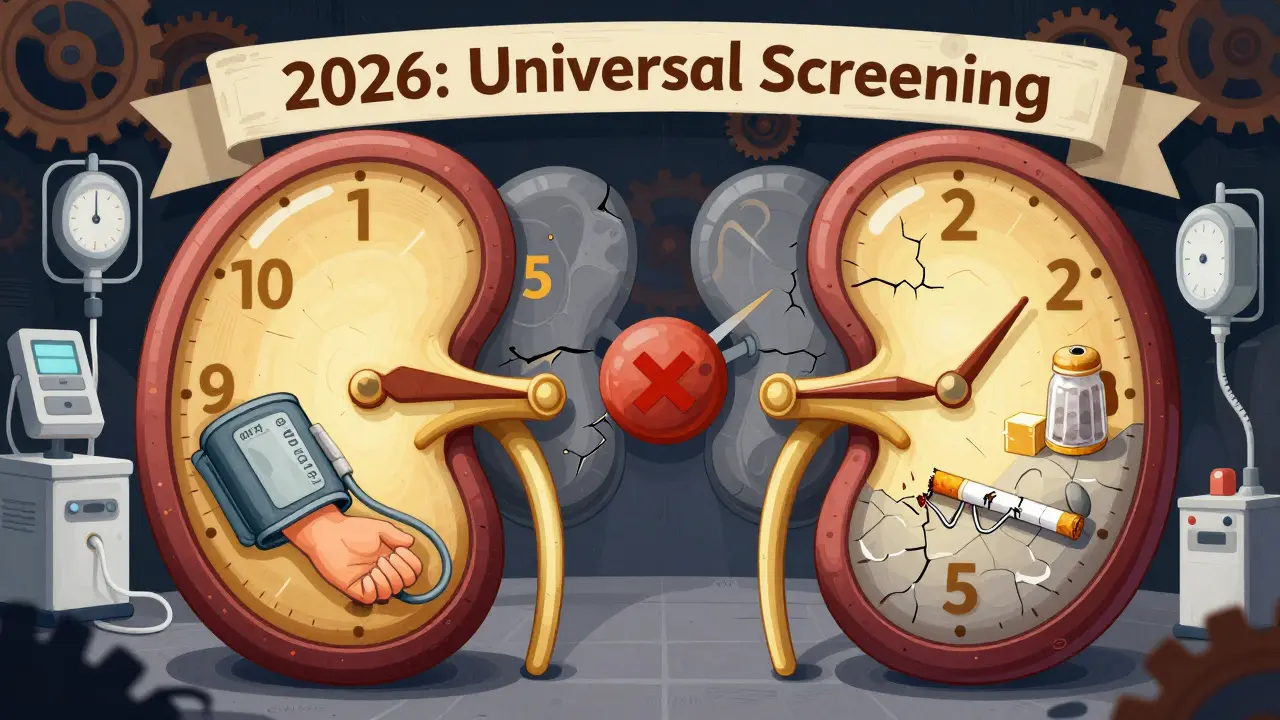
What’s Changing in 2026
The field is moving fast. In 2023, the FDA cleared the first AI tool-NephroSight by Renalytix-that analyzes 32 data points (blood tests, age, BMI, medications, etc.) to predict who’s at risk for CKD before eGFR drops. It’s not perfect, but it’s a step toward catching problems earlier than ever.
Also, race adjustment in eGFR calculations is being phased out. For years, Black patients had their eGFR artificially boosted by 15-20%, making their kidney function look better than it was. That masked early damage. New formulas without race adjustments are now being adopted. Early data shows this could increase early detection in African Americans by 12.3%.
The Biden administration’s 2023 Executive Order on Kidney Health includes $150 million to roll out mandatory dual-testing in Federally Qualified Health Centers by 2026. That means millions of low-income patients-many of whom are at highest risk-will finally get screened.
And in 2025, the FDA plans to approve point-of-care uACR devices. Imagine getting your urine test result in 10 minutes during a routine checkup, not waiting weeks. That could boost screening rates by 40% in primary care.
What You Can Do Right Now
If you have diabetes, high blood pressure, heart disease, or a family history of kidney failure, ask your doctor for two tests: eGFR and uACR. Don’t wait for them to bring it up. Say: “I’d like to check my kidney health. Can we do both tests?”
If you’re over 60, even without other risk factors, get screened every year. CKD risk climbs with age.
If you’re told you have stage 1 or 2 CKD, don’t panic. You’re not doomed. You’re in the window where lifestyle and medication can stop this in its tracks. Work with your doctor. Track your numbers. Stick to your plan.
And if you’ve been told your kidneys are fine because your creatinine was normal? Ask if your uACR was checked. If not, request it. That one test could change your future.
Can you have chronic kidney disease without symptoms?
Yes. In fact, most people with early-stage CKD have no symptoms at all. Fatigue, swelling, or nausea usually appear only after significant kidney damage has occurred. That’s why testing is critical-even if you feel fine.
Is CKD the same as kidney failure?
No. CKD is a broad term that includes all stages of kidney damage, from mild to severe. Kidney failure is stage 5 CKD, where the kidneys can no longer support life without dialysis or transplant. Most people with CKD never reach kidney failure if caught early and managed well.
Why do I need both eGFR and uACR? Can’t one test be enough?
No. eGFR tells you how well your kidneys filter, but it can be misleading if you have low muscle mass or are elderly. uACR detects kidney damage from protein leakage, even when eGFR is normal. Together, they give a complete picture. Relying on just one misses up to 40% of early cases.
Does having high blood pressure mean I’ll get CKD?
Not necessarily, but it greatly increases your risk. High blood pressure damages the tiny blood vessels in the kidneys over time. If you have hypertension, annual screening with eGFR and uACR is essential. Controlling your pressure to under 130/80 can cut your risk of progression by nearly one-third.
Can lifestyle changes really reverse CKD?
They can’t repair scarred tissue, but they can stop further damage. In stage 1 and 2 CKD, strict blood pressure control, blood sugar management, a low-sodium diet, and avoiding kidney-toxic drugs can slow or even halt progression. Some people stabilize for decades. The goal isn’t reversal-it’s prevention of worsening.
Is CKD screening covered by insurance?
Yes, for people at high risk. Medicare and most private insurers cover annual eGFR and uACR tests for those with diabetes, hypertension, obesity, or a family history of kidney disease. Even if you’re not symptomatic, if you’re in a high-risk group, the tests should be covered at no cost.