When your stomach hurts, you feel bloated, or you’re rushing to the bathroom more than usual, it’s easy to assume it’s just IBS. But what if it’s something more serious? Many people confuse Irritable Bowel Syndrome (IBS) with Inflammatory Bowel Disease (IBD) because the symptoms overlap - cramping, diarrhea, gas, bloating. But they’re not the same. One is a functional disorder with no visible damage. The other is a structural disease that can tear your gut apart. Knowing the difference isn’t just about labels - it’s about getting the right treatment, avoiding unnecessary stress, and recognizing when you need urgent care.
IBS: Your Gut Is Working, But It’s Misfiring
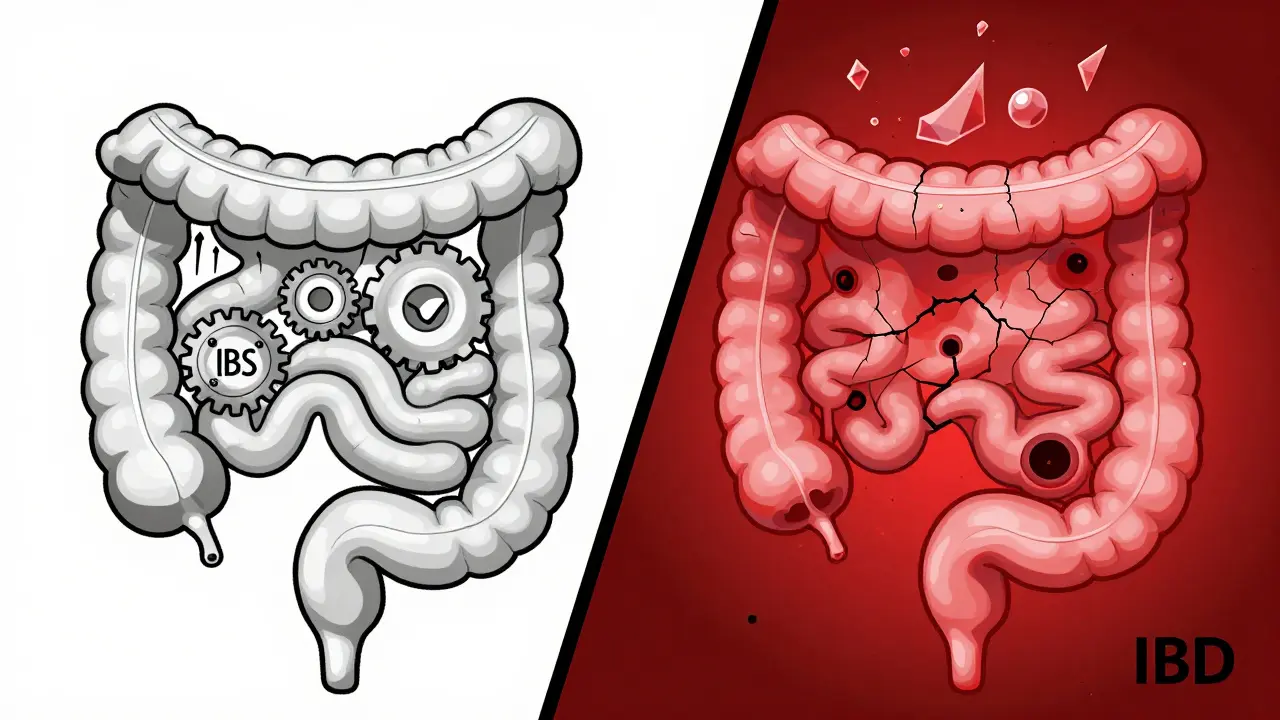
IBS isn’t caused by inflammation, ulcers, or damaged tissue. Your colon looks perfectly normal on a colonoscopy. No blood tests show signs of disease. No scans reveal abnormalities. Yet you still feel awful. That’s because IBS is a functional disorder - meaning your gut’s wiring is off. It’s like a car with a faulty sensor: everything looks fine under the hood, but the engine sputters.
The Rome IV criteria, used by doctors worldwide since 2016, define IBS as recurrent abdominal pain at least one day a week for three months, linked to bowel movements or changes in stool frequency or form. About 76% of people with IBS report constant bloating. Nearly half see mucus in their stool. Three out of five experience worse symptoms after eating. For many, it’s triggered by stress, certain foods, or hormonal shifts - especially in women, who make up 65% of IBS cases.
Here’s the key: IBS doesn’t cause bleeding, weight loss, or fever. If you’re losing weight without trying, running a low-grade fever, or seeing blood in your stool, you’re not dealing with typical IBS. Those are red flags. And they point to something else - likely IBD.
IBD: When Your Immune System Attacks Your Gut
IBD is not a glitch. It’s a war. Your immune system turns on your own digestive tract, causing chronic inflammation. This isn’t temporary irritation - it’s ongoing damage. Two main types exist: Crohn’s disease, which can affect any part of the GI tract from mouth to anus, and ulcerative colitis, which targets only the colon and rectum.
Doctors see the damage. Endoscopies show open sores, deep ulcers, and inflamed, bleeding tissue. Biopsies confirm immune cell invasion. Blood tests reveal elevated CRP and fecal calprotectin - markers of active inflammation. In 92% of ulcerative colitis cases, blood appears in stool. In 15% of Crohn’s patients, you’ll see black, tarry stools from upper GI bleeding. About 65% of IBD patients lose weight during flares. Fever is common in moderate to severe cases.
And it doesn’t stop in the gut. IBD can cause joint pain, eye inflammation (uveitis), skin rashes like erythema nodosum, and liver problems. These are called extraintestinal manifestations. They’re proof this isn’t just a digestive issue - it’s a systemic autoimmune condition.
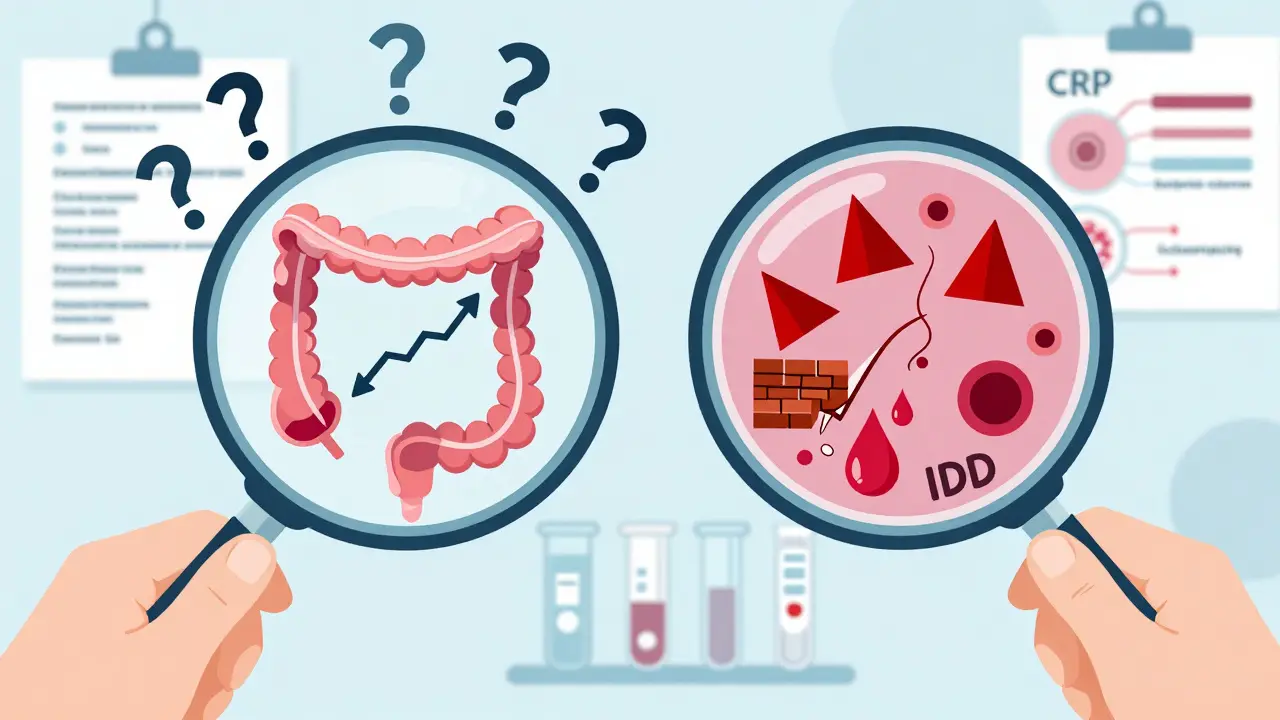
How Doctors Tell Them Apart
There’s no single test for IBS. Diagnosis is a process of elimination. If your blood work, stool tests, colonoscopy, and imaging come back normal - and you have the right symptoms - you’re likely diagnosed with IBS. Doctors call this a “diagnosis of exclusion.”
For IBD, the path is the opposite. Doctors don’t rule things out - they look for proof of damage. A colonoscopy with biopsy is the gold standard. If they see inflammation, crypt abscesses, or granulomas (tiny clusters of immune cells), it’s IBD. MRI enterography can spot strictures or fistulas in Crohn’s patients. Blood tests showing high CRP or fecal calprotectin above 250 µg/g are strong indicators.
Alarm symptoms? They’re your signal to push for more testing. If you have:
- Rectal bleeding or black stools
- Unexplained weight loss
- Fever without infection
- Anemia
- Family history of IBD or colon cancer
- you need a full workup. These aren’t IBS symptoms. They’re IBD red flags.
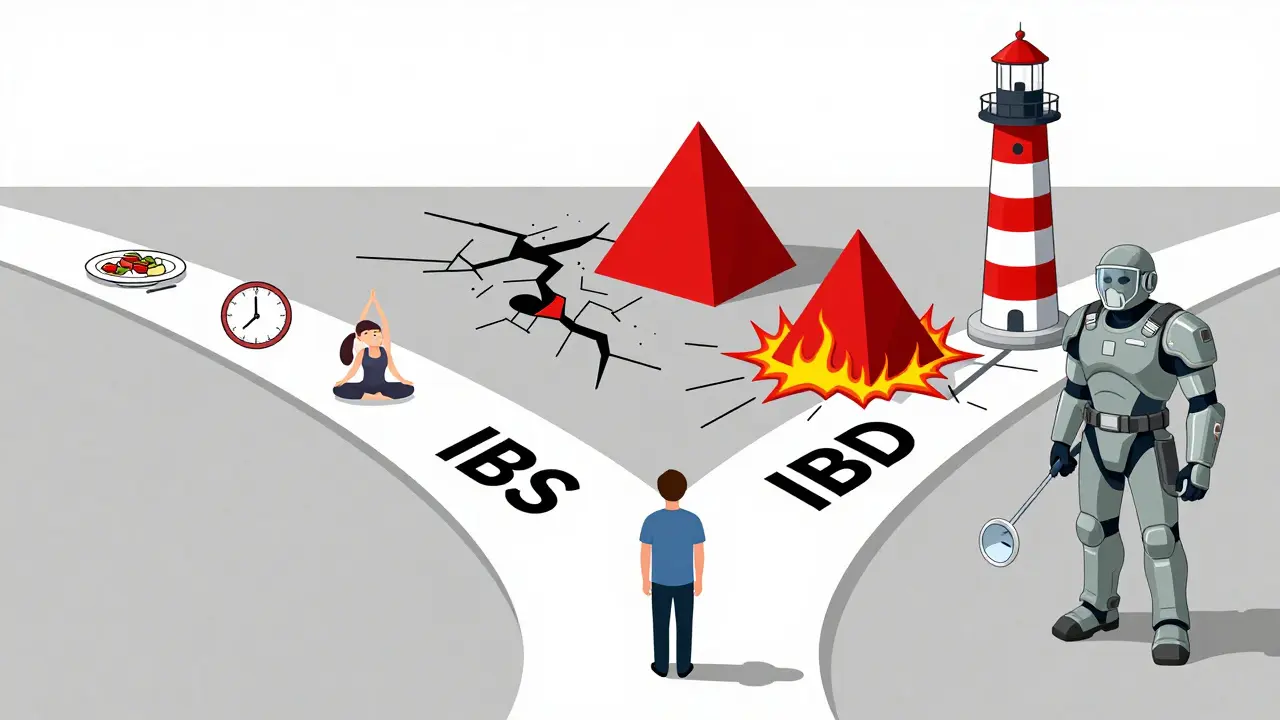
Treatment: Fixing the System vs. Calming the Noise
IBS treatment focuses on managing signals - not repairing tissue. The low-FODMAP diet helps 76% of patients reduce bloating and pain. Low-dose antidepressants like amitriptyline can calm nerve sensitivity in the gut, cutting pain by half in 60% of cases. Medications like eluxadoline target diarrhea-predominant IBS, helping 35-40% of patients.
IBD treatment is about stopping the attack. Drugs like infliximab block tumor necrosis factor (TNF), a key inflammation trigger. In 50-60% of Crohn’s patients, it brings symptoms into remission within 14 weeks. Steroids like prednisone work fast for flares, but they’re not safe long-term. Newer biologics like vedolizumab target only gut-specific immune cells, reducing side effects.
Here’s something many don’t know: you can have both. About 22-35% of people with IBD in remission still meet IBS criteria. Their gut is healed enough to stop bleeding and inflammation - but the nerves are still hypersensitive. That’s why some IBD patients still get bloating or cramps even when their disease is controlled.
Long-Term Risks: What’s at Stake?
IBS doesn’t turn into cancer. It doesn’t cause bowel obstructions or fistulas. It doesn’t shorten your life. But it can wreck your quality of life. Studies show IBS patients are willing to give up coffee, sex, or even their phone to be symptom-free. It’s exhausting. It’s isolating. But it’s not dangerous.
IBD is different. Chronic inflammation increases cancer risk. After 10 years of pancolitis (ulcerative colitis affecting the entire colon), your risk of colorectal cancer rises by 2% each year. Untreated Crohn’s can lead to strictures - narrowed sections of intestine - that block food. Fistulas - abnormal tunnels between organs - can cause infections and abscesses. Toxic megacolon, a rare but life-threatening dilation of the colon, happens in 2-4% of severe ulcerative colitis cases.
These aren’t hypotheticals. They’re documented outcomes. That’s why IBD requires lifelong monitoring, regular colonoscopies, and sometimes surgery.
What You Should Do Next
If you’ve been told you have IBS but still have bleeding, weight loss, or fever - get a second opinion. Don’t assume it’s “just stress.” If you have IBD and still get daily cramps and bloating after remission, talk to your doctor about IBS overlap. You’re not imagining it.
Start with a basic blood test and stool calprotectin. If those are normal and you have typical IBS symptoms, you’re likely on the right track. If they’re high, or if you have alarm symptoms, push for a colonoscopy. Early detection of IBD changes everything.
And remember: IBS doesn’t become IBD. That’s a myth. But IBD can hide behind IBS-like symptoms - especially in early stages. Don’t delay testing because you think it’s “just IBS.”
Can IBS turn into IBD?
No, IBS cannot turn into IBD. They are two completely different conditions. IBS is a functional disorder with no structural damage or inflammation. IBD is an autoimmune disease that causes physical damage to the intestinal lining. While you can have both at the same time - especially if you have IBD in remission - one does not progress into the other.
Is blood in stool a sign of IBS?
No, blood in the stool is not a symptom of IBS. If you see red blood in your toilet, on toilet paper, or in your stool, it’s a red flag for IBD, colorectal cancer, or another serious condition. IBS causes changes in bowel habits and discomfort, but never bleeding. Seek medical attention immediately if you notice blood.
Can stress cause IBD?
Stress doesn’t cause IBD, but it can trigger flares. IBD is an autoimmune disease with genetic and environmental roots - not psychological. However, stress can worsen inflammation and make symptoms harder to control. Managing stress is part of IBD care, but it won’t prevent or cure the disease.
What’s the best test to tell IBS from IBD?
The best test is a colonoscopy with biopsy, combined with blood and stool tests. Fecal calprotectin above 250 µg/g strongly suggests IBD. Normal results, along with typical IBS symptoms and no alarm signs, support an IBS diagnosis. Imaging like MRI enterography may also be used if Crohn’s is suspected.
Can IBD be cured?
There is no cure for IBD yet, but it can be managed effectively. Many patients achieve long-term remission with biologics, immunosuppressants, or surgery. The goal is to stop inflammation, heal the gut lining, and prevent complications. Some people live decades without symptoms. IBS, while not curable, often improves significantly with diet, stress management, and targeted medications.
Are there foods that help IBS but hurt IBD?
Yes. The low-FODMAP diet helps most IBS patients by reducing gas and bloating. But for IBD patients in active flare, high-fiber or high-fat foods can worsen symptoms - even if they’re low-FODMAP. During flares, IBD patients often need low-residue diets, not high-fiber ones. What helps one condition can irritate the other. Always tailor diet to your diagnosis and current disease activity.



Jeane Hendrix January 6, 2026
Okay but can we talk about how the low-FODMAP diet is basically a food prison? I tried it for 3 months, eliminated everything that tasted good, and still got bloated after eating a single cucumber. Like... what even is my gut? I feel like I'm being punished for existing.
Tom Swinton January 7, 2026
I just want to say-this post? This is the kind of clarity people need when they’re stuck in that limbo between ‘it’s all in my head’ and ‘oh god I might be dying.’ I’ve had both IBS and Crohn’s in my family, and I’ve seen how fast doctors dismiss bloating as stress-until someone ends up in the ER with a perforated colon. Please, if you’re reading this and you’ve been told ‘it’s just IBS’ but you’re losing weight or bleeding-don’t wait. Push. Hard. Because your gut isn’t being dramatic-it’s screaming.
Venkataramanan Viswanathan January 7, 2026
While the medical distinctions are well-articulated, I must emphasize that in many developing regions, access to colonoscopies or fecal calprotectin testing remains a luxury. For many, symptom-based diagnosis remains the only option, and misclassification is common. Awareness must extend beyond Western medical frameworks to reach those without resources.
Kelly Beck January 8, 2026
Y’all, I’ve been living with IBD for 12 years and I still get emotional reading posts like this. 🥹 The fact that you explained how IBS can linger even after IBD is in remission? That’s the missing piece for SO MANY of us. I thought I was failing at healing because I still got bloated after salads-turns out my nerves were just still jacked up. You’re not alone. And yes, you’re not imagining it. Keep advocating for yourself. You’ve got this. 💪❤️
Katie Schoen January 10, 2026
So let me get this straight-IBS is ‘your gut has anxiety’ and IBD is ‘your immune system is literally at war in your intestines’? Cool. So IBS is the overreactive roommate, and IBD is the arsonist who set the whole building on fire. And yet somehow, people still think IBS is ‘just stress.’ 🙄
Stuart Shield January 11, 2026
It’s like comparing a misfiring spark plug to a blown engine block. One’s a nuisance, the other’s a catastrophe. I’ve had both, and I can tell you-the moment you start seeing blood in your stool, you don’t google ‘IBS remedies.’ You book the colonoscopy like your life depends on it-because it does. This isn’t a ‘maybe’ situation. It’s a ‘call your doctor now’ situation.
Joann Absi January 13, 2026
IBS is a product of woke culture. People are so obsessed with ‘listening to their body’ that they’ve turned normal digestion into a trauma narrative. Meanwhile, real diseases like IBD get drowned out by people who think their gas is a medical emergency. Wake up. Your gut isn’t a sacred temple-it’s a pipe. Stop anthropomorphizing your colon.
Gabrielle Panchev January 14, 2026
Wait-so you’re saying IBS can’t turn into IBD… but then you say 22-35% of IBD patients in remission still meet IBS criteria? That sounds like a contradiction. If IBD is healed, but the symptoms are identical to IBS, then aren’t you just re-labeling the same condition? Or is this just a way for pharma to sell more meds to people who already have IBD? I’m not buying it.