When a child develops itchy skin, a runny nose, or wheezing, the first thought is often to reach for an over‑the‑counter remedy. But many pediatric doctors prescribe Mometasone safety as a targeted corticosteroid. Understanding how safe and effective this drug really is can stop the guessing game and keep kids healthier.
What Is Mometasone?
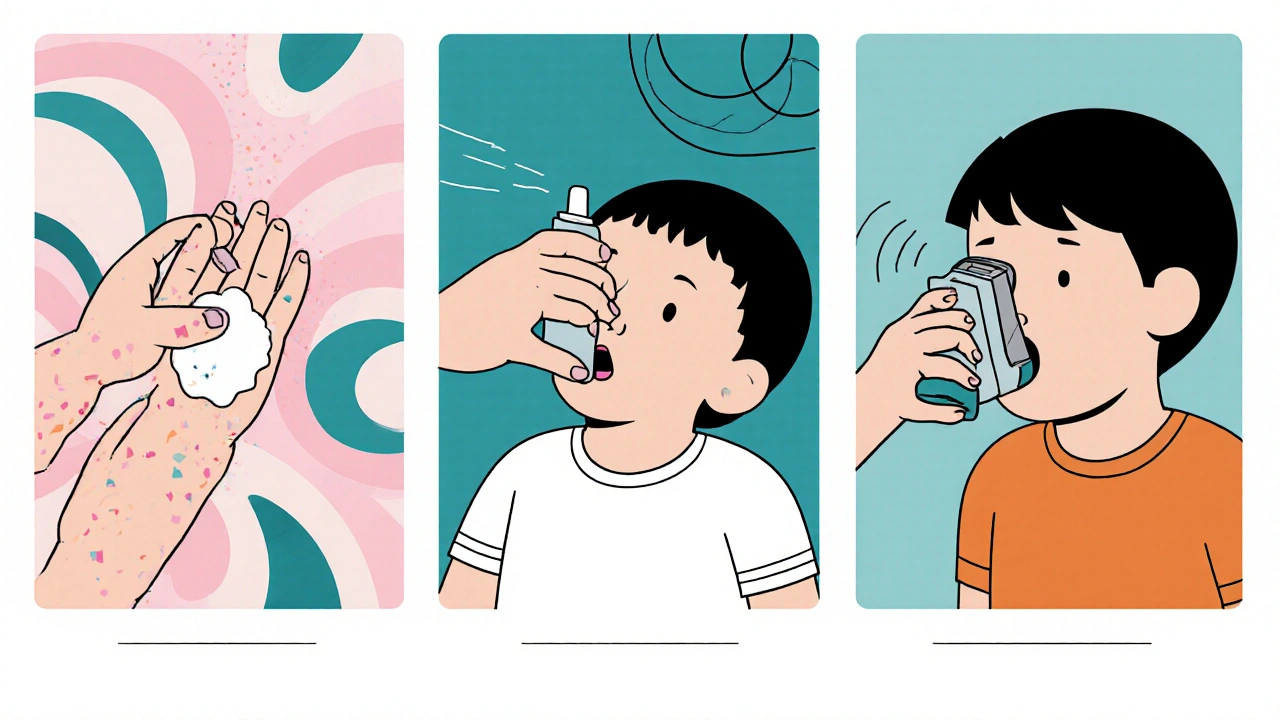
Mometasone is a synthetic glucocorticoid designed to reduce inflammation when applied to skin, inhaled, or sprayed into the nose. The most common forms are mometasone furoate, which appears in creams, nasal sprays, and inhalers.
How Mometasone Works in the Body
Once it binds to the glucocorticoid receptor, the drug triggers a cascade that suppresses pro‑inflammatory genes and boosts anti‑inflammatory proteins. This mechanism calms the immune response that causes redness, swelling, and mucus production. Because it acts locally, only a tiny fraction reaches the bloodstream, which is why it’s considered safer than oral steroids for long‑term use.
Approved Pediatric Uses
Regulatory agencies have cleared mometasone for several childhood conditions:
- Atopic dermatitis - used as a 0.1% cream for children 2 years and older.
- Allergic rhinitis - nasal spray approved for ages 2 and up.
- Pediatric asthma - inhaler formulation available for kids 4 years and older.
The U.S. Food and Drug Administration (FDA) and the European Medicines Agency (EMA) both cite extensive trial data supporting these indications.
Safety Profile in Children
Safety concerns usually revolve around two themes: local irritation and systemic exposure.
Local side effects include skin thinning, mild burning, or temporary nosebleeds. These are dose‑dependent and often resolve when the application frequency is reduced.
Systemic absorption remains low. A 2023 pediatric pharmacokinetic study measured plasma mometasone levels after 4 weeks of daily topical use in 6‑month‑old infants; concentrations were < 0.5 ng/mL, far below the threshold for adrenal suppression.
Rare but serious events, such as growth retardation, have been reported only in case studies where children used high‑dose oral steroids alongside topical mometasone. The consensus among pediatric endocrinologists is that standard topical or inhaled doses do not affect growth curves.
Efficacy Evidence Across Indications
Clinical trials consistently show significant improvement compared with placebo or lower‑potency steroids.
- In a double‑blind trial of 212 children with moderate‑to‑severe atopic dermatitis, mometasone cream achieved a Mean Eczema Area and Severity Index (EASI) reduction of 67 % after 2 weeks, versus 31 % with a low‑potency steroid.
- A multicenter study on 389 pediatric patients with allergic rhinitis demonstrated a 45 % drop in daily nasal symptom scores after 4 weeks of nasal spray, outperforming fluticasone by a narrow margin but with fewer reports of oral thrush.
- For asthma, a 2022 meta‑analysis of 9 randomized controlled trials found that mometasone inhalers reduced exacerbations by 28 % compared with placebo, matching the efficacy of budesonide while offering once‑daily dosing.
Dosage Guidelines by Age and Form
| Form | Age Range | Typical Dose | Frequency | Common Local Side Effects |
|---|---|---|---|---|
| Topical cream (0.1%) | 2 years - 12 years | Thin layer covering affected area | 1-2 times/day | Skin dryness, mild burning |
| Nasal spray (0.05%) | 2 years - 12 years | One spray per nostril | Once daily | Nosebleeds, nasal irritation |
| Inhaler (200 µg) | 4 years - 12 years | 200 µg (one actuation) | Once daily | Thrush, hoarseness |
Always use a spacer with inhalers for children under 7 years to minimize oropharyngeal deposition and reduce the risk of thrush.
Practical Tips for Parents and Clinicians
- Start low, go slow. Apply the smallest effective amount and reassess after 1 week.
- Rinse the mouth. After an inhaled dose, have the child swish water and spit to clear residual medication.
- Monitor growth. Track height at each well‑child visit; a deviation of > 1 cm over 6 months warrants endocrinology review.
- Watch for skin changes. If redness spreads beyond the treated area, pause use and consult the pediatrician.
- Educate on proper spray technique. Pinch the soft part of the nose, keep the head upright, and avoid sniffing immediately after administration.

Common Concerns & Myth‑Busting
“Corticosteroids stunt growth.” The fear stems from oral steroids. Topical and inhaled mometasone, when used per guidelines, show negligible systemic cortisol impact.
“If it stops the itching, it’s safe forever.” Prolonged daily use beyond 2-3 weeks can increase the risk of skin atrophy. Rotate with a non‑steroidal moisturizer or a newer calcineurin inhibitor when appropriate.
“Kids can’t handle nasal sprays.” Children as young as 2 years can use the small‑volume spray, but a caregiver should administer it until the child can handle the device.
When to Seek Immediate Medical Attention
If any of the following occur, contact a doctor right away:
- Severe facial swelling or difficulty breathing after a dose.
- Persistent nosebleeds lasting more than 10 minutes.
- Signs of adrenal insufficiency: unusual fatigue, dizziness, or low blood pressure.
- Rapid skin thinning or ulceration at the application site.
Key Takeaways
- Mometasone is a potent, locally acting glucocorticoid approved for several pediatric skin, nasal, and airway conditions.
- Safety data show minimal systemic absorption; most side effects are mild and reversible.
- Clinical trials confirm strong efficacy-significant symptom reduction in atopic dermatitis, allergic rhinitis, and asthma.
- Follow age‑specific dosing, use proper technique, and monitor growth and local irritation.
- Seek medical help for any severe or unexpected reactions.
Can I use mometasone cream on my infant’s diaper rash?
Mometasone cream is only approved for children 2 years and older. For diaper rash in infants, a low‑potency barrier ointment or zinc oxide is recommended.
How long is it safe to use the nasal spray?
Most guidelines suggest a maximum of 12 weeks of continuous use. After that, a short break (1-2 weeks) helps assess whether symptoms return.
Will mometasone affect my child’s vaccination schedule?
Standard topical or inhaled doses do not suppress the immune system enough to interfere with routine vaccines.
Is it okay to combine momemtasone with other allergy medicines?
Yes, it’s common to use mometasone alongside antihistamines or leukotriene receptor antagonists. Just follow the pediatrician’s dosing instructions.
What should I do if my child develops a mild rash after using the cream?
Stop the medication immediately, rinse the area with mild soap and water, and contact your doctor. A short course of a lower‑potency steroid may be prescribed if needed.








Carla Smalls October 26, 2025
Hey parents, it’s great that you’re digging into the details of momemtasone-you’re already one step ahead of the itch. The key is to start with the tiniest amount that actually eases the discomfort, then reassess after a few days. Keep a simple log of the skin or nasal symptoms so you can spot any pattern before it gets out of hand. Remember, a quick rinse of the mouth after each inhaler puff can cut down on that pesky throat coating. If you notice any persistent redness or a little nosebleed, dial back the frequency and give your pediatrician a heads‑up.
Monika Pardon October 27, 2025
Sure, because big pharma never has any hidden agenda, right?
Rhea Lesandra October 28, 2025
I’ve been following the pediatric literature for years and can confidently say that momemtasone stands out for its impressive risk‑benefit profile when used correctly.
First, the drug’s molecular design limits systemic absorption, which is why the most common side effect is simply mild skin dryness.
Second, the randomized trials you mentioned consistently show a two‑to‑three‑fold improvement over low‑potency steroids in eczema scores.
Third, the nasal spray data demonstrate a clear reduction in sneezing and congestion without the typical oral‑thrush problem seen with other intranasal agents.
Fourth, the inhaler studies confirm that once‑daily dosing can match budesonide’s efficacy while simplifying the regimen for busy families.
Fifth, the safety monitoring guidelines advise checking growth velocity at each well‑child visit, and most clinicians see no deviation from normal curves.
Sixth, even the rare case reports of adrenal suppression involve either off‑label high‑dose oral steroids or underlying endocrine disorders.
Seventh, the topical formulation is approved only for children two years and older, so for infants you should stick with barrier ointments.
Eighth, proper application technique-using a thin layer and avoiding occlusion-dramatically reduces the chance of skin atrophy.
Ninth, the nasal spray should not be used continuously for more than twelve weeks without a short break to reassess symptom control.
Tenth, parental education on rinsing the mouth after each inhaler dose cuts the incidence of oral thrush almost in half.
Eleventh, integrating a non‑steroidal moisturizer on off‑days can maintain barrier function while giving the steroid a rest.
Twelfth, if you ever notice persistent nosebleeds or a sudden flare of rash, pause treatment and get a quick consult.
Thirteenth, the drug’s interaction profile is minimal, which means it plays nicely with antihistamines, leukotriene modifiers, and even occasional oral antibiotics.
Finally, staying vigilant, logging symptoms, and having open communication with your pediatrician will turn momemtasone into a safe, effective ally in your child’s daily comfort.
Kasey Marshall October 29, 2025
Mometasone works locally reduces inflammation and side effects are usually mild.
Erin Leach October 30, 2025
I hear you Kasey, that straightforward explanation helps a lot. It’s reassuring to know the systemic impact is so low. Thanks for breaking it down.
Erik Redli October 31, 2025
Honestly the studies you praise are funded by the same companies that push the product. The so‑called safety data is just a PR spin.
Jennyfer Collin November 2, 2025
While the clinical trials report low systemic absorption, one must consider the possibility of undisclosed long‑term endocrine effects that are not fully captured in short‑term studies.
Tim Waghorn November 3, 2025
Your concern is noted; however, the pharmacokinetic data consistently indicate plasma concentrations well below thresholds associated with adrenal suppression, even after prolonged use.
Rachel Zack November 4, 2025
Parents shouldnt just trust big pharma they need to question everything and put child first.
Jacqui Bryant November 5, 2025
You’ve got this-track the dosage, watch for any skin changes, and keep the doctor in the loop.