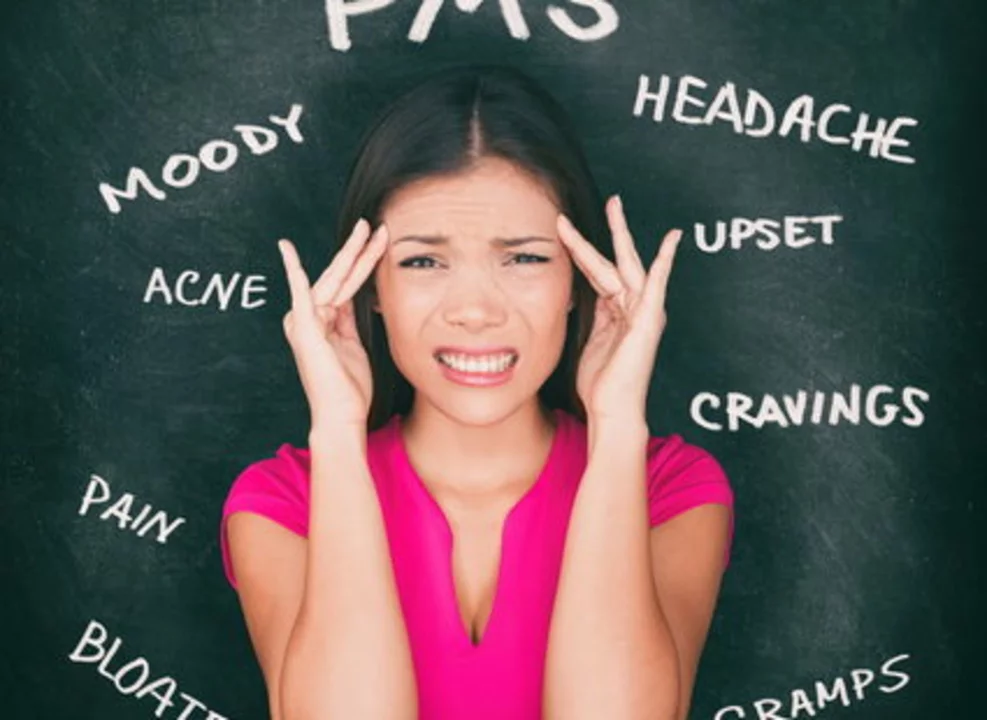
Understanding Premenstrual Syndrome
Premenstrual Syndrome (PMS) is a common condition that affects women of reproductive age. It is characterized by a variety of physical, emotional, and behavioral symptoms that typically occur in the days leading up to menstruation. Some of the most common symptoms include bloating, mood swings, irritability, fatigue, and breast tenderness. These symptoms can vary in intensity and duration, and they can significantly impact a woman's daily life.
As a woman myself, I can attest to the challenges PMS can bring. It's important to understand that PMS is a real, legitimate health issue that deserves attention and care. By knowing what to expect and how to manage symptoms, we can better navigate this monthly occurrence and maintain a higher quality of life.
Recognizing Menopause
Menopause is another significant stage in a woman's life, marking the end of her reproductive years. This natural biological process usually occurs between the ages of 45 and 55, with the average age being 51. Menopause is defined as the point when a woman has not had a menstrual period for 12 consecutive months. It is a normal part of aging, but it can also bring about various physical and emotional changes that may be challenging to navigate.
Some common symptoms of menopause include hot flashes, night sweats, mood changes, weight gain, and sleep disturbances. It's essential to recognize these symptoms and understand how they may impact our daily lives, as well as seek support and treatment when necessary.
How PMS and Menopause Symptoms Can Overlap
While PMS and menopause are distinct stages in a woman's life, they share some similarities in terms of symptoms. Both can cause mood swings, irritability, fatigue, and sleep disturbances. This can sometimes make it difficult for women to differentiate between the two conditions, especially during the perimenopausal period when hormone levels fluctuate more dramatically.
As someone who has experienced both PMS and menopause symptoms, I can attest to the confusion and frustration that can arise. However, it's important to remember that these experiences are a normal part of the female life cycle and that there are ways to manage and cope with these symptoms.
Managing PMS Symptoms
There is no one-size-fits-all solution for managing PMS symptoms, as each woman's experience is unique. However, there are some general strategies that can help alleviate the physical and emotional discomfort associated with PMS. These include maintaining a healthy diet, engaging in regular physical activity, practicing stress reduction techniques, and getting adequate sleep.
Additionally, over-the-counter medications like pain relievers and anti-inflammatory drugs can help alleviate physical symptoms like cramps and headaches. For more severe cases, hormonal treatments like birth control pills may be prescribed to help regulate hormone levels and alleviate PMS symptoms.
Managing Menopause Symptoms
Similar to PMS, there is no one-size-fits-all approach to managing menopause symptoms. However, there are several strategies that can help alleviate the discomfort and challenges associated with this life stage. Lifestyle modifications like maintaining a healthy diet, engaging in regular physical activity, and practicing stress reduction techniques can all help to manage symptoms like hot flashes, mood swings, and sleep disturbances.
For more severe symptoms, hormone replacement therapy (HRT) may be prescribed by a healthcare professional. HRT involves taking supplemental hormones to help regulate hormone levels and alleviate symptoms. It's important to consult with a healthcare provider to determine if HRT is the right option for you, as there are potential risks and benefits to consider.
Support and Resources for Women Experiencing PMS and Menopause
As women, it's important that we support and empower one another during these challenging times in our lives. Sharing our experiences with friends, family members, or support groups can help to normalize these experiences and provide valuable advice and encouragement. Additionally, seeking professional support from healthcare providers, therapists, or counselors can help us navigate these life stages with greater ease and understanding.
There are also numerous online resources available that provide information, advice, and support for women experiencing PMS and menopause. Some of my personal favorites include websites like the Office on Women's Health, the North American Menopause Society, and the American College of Obstetricians and Gynecologists. By educating ourselves and seeking support, we can better understand and manage the challenges associated with PMS and menopause.







Aurora Morealis May 13, 2023
Premenstrual symptoms can often be eased by keeping a balanced diet rich in whole grains, fruits, and vegetables. Regular light exercise such as walking or yoga helps stabilize mood swings and reduces fatigue. Adequate sleep of seven to eight hours each night supports hormonal balance. Stress‑management techniques like deep breathing or meditation are also beneficial. If over‑the‑counter pain relievers are needed, using them as directed can provide additional relief.
Sara Blanchard May 30, 2023
It’s important to remember that every woman’s experience with PMS or menopause is unique, and we should celebrate that diversity. Creating an inclusive environment where women feel safe to share their stories can reduce stigma. Peer support groups, both online and in‑person, often provide practical tips that complement medical advice. Access to culturally sensitive resources ensures that language barriers do not prevent anyone from getting help. By listening and offering empathy, we build a stronger community for all.
Anthony Palmowski June 17, 2023
Wow!!! You’ve got some solid advice there, but let’s be real-most people never actually follow it!!!
Reading about diet and yoga is nice, but life is busy, work is stressful, and who has time for meditation???
Instead of just preaching, why not give us quick hacks that fit a chaotic schedule???
Bottom line: if you want results, you need to actually commit, not just nod and say “maybe”.
Jillian Rooney July 4, 2023
Women shouldnt tolerate these symptons and must demand better care.
Rex Peterson July 21, 2023
The transition from reproductive vitality to the post‑menopausal phase invites a profound contemplation of the human condition. In ancient philosophy, the concept of *midlife* was often linked to a period of introspection and renewal. Modern medicine confirms that hormonal fluctuations are not merely biological events but also psychosocial catalysts. When a woman recognizes the overlap between PMS and menopause, she confronts the paradox of continuity and change. Such awareness can foster resilience, as the mind learns to navigate discomfort with measured equanimity. Dietary considerations, including adequate calcium and vitamin D, serve as tangible anchors amidst hormonal turbulence. Physical activity, especially low‑impact aerobic exercise, promotes both vascular health and emotional stability. Sleep hygiene, encompassing regular bedtime routines and limiting stimulants, mitigates the insomnia often reported in late‑stage perimenopause. Therapeutic dialogues with health professionals enable personalized strategies that respect individual values. Ethical considerations arise when prescribing hormone replacement therapy, demanding a balance between benefit and risk. Cultural narratives about aging influence how women internalize their symptoms and seek support. By fostering open discourse, societies can dismantle the stigma that frequently surrounds women’s health transitions. Philosophically, embracing the impermanence of bodily states aligns with the broader Stoic principle of accepting what lies beyond our control. Nonetheless, proactive engagement in self‑care reflects an exercise of agency that empowers rather than diminishes. Ultimately, the interwoven experience of PMS and menopause underscores the enduring capacity of women to adapt, thrive, and contribute meaningfully throughout all stages of life.
Candace Jones August 8, 2023
Consistent movement, such as brisk walking for thirty minutes most days, can lower the frequency of hot flashes.
Incorporating magnesium‑rich foods like nuts and leafy greens may ease muscle tension during PMS.
Staying hydrated supports overall circulation and can reduce bloating.
If symptoms become disruptive, consulting a healthcare provider about non‑hormonal options is advisable.
Remember to track your symptoms in a journal to identify patterns that respond to specific lifestyle changes.
Robert Ortega August 25, 2023
That’s a practical approach; keeping a symptom log really helps pinpoint triggers.
Balancing activity with rest ensures the body isn’t overtaxed.
Overall, small sustainable habits often yield the best long‑term results.
Elizabeth Nisbet September 11, 2023
Great tips! Keep experimenting with what feels right for your body.
Don’t hesitate to lean on friends or online communities for extra motivation.
Small victories add up, so celebrate each step forward.
You’ve got this.