Heartburn can sneak up on you after your favorite spicy meal or just from lying down at the wrong time, turning a good night into a battle with chest pain and a sour taste you can’t ignore. For millions, those moments send them reaching for a little purple pill: Prilosec. You’ve probably seen ads on TV promising relief, but how much do you actually know about what you’re swallowing?
What is Prilosec, and How Does It Actually Work?
Prilosec’s real name at the pharmacy is omeprazole, and it belongs to a group called proton pump inhibitors—PPIs for short. The job of a PPI isn’t just to mask symptoms like antacids do. Instead, omeprazole blocks an enzyme in your stomach wall that actually produces acid. Less acid means less burn, and for most with stubborn heartburn, it feels like a rescue.
Prilosec doesn’t work the instant you take it. After you swallow the pill, your body needs a day or so to get the medication working as designed. Each day you take it, the acid production stays shut down, which is why people with chronic reflux take it every morning. One super important fact: it’s not a magic fix for everyone. It’s best for folks with frequent, long-lasting symptoms. If you’re someone who just gets mild heartburn once a month, popping Prilosec probably isn’t the answer—it’s more of a long-game pill.
The brand Prilosec first hit the U.S. market in 1989, exploding in popularity. Today, it comes in both prescription and over-the-counter versions. OTC Prilosec usually comes as 20 mg tablets. Doctors sometimes prescribe double that dose in more severe cases (usually 40 mg).
Here’s a fun fact: the active ingredient in Prilosec, omeprazole, was the first member in the whole PPI family. Since then, several other copycats (like Nexium, also known as esomeprazole, and Prevacid, or lansoprazole) have followed. What makes Prilosec unique is that it’s still one of the most studied and trusted choices in the lineup.
The acid blocking isn’t permanent, though. Your stomach pumps make new little proton pumps every day, so when you stop the medication, acid comes back. That’s why Prilosec isn’t meant to be taken forever for most problems. Usually, doctors suggest 14 days at a time, up to three times a year if you’re using the OTC version. Prescription use can go longer if there’s a medical reason behind it (like ulcers or damage in your esophagus).
Here’s something you might not realize: Prilosec isn’t just for heartburn. Doctors prescribe it for stomach ulcers, damage to the esophagus from too much acid (called erosive esophagitis), and even certain rare syndromes that cause massive acid production.
Real-World Uses: When (and When Not) to Grab Prilosec
Tablets say “for frequent heartburn,” but what does that mean? If you’re dealing with burning chest pain two or more days a week, the FDA says you’re its target customer. The catch? If your symptoms are new, or have changed, see your doctor—sometimes heartburn masks things way more serious, like a heart attack or even cancer (not trying to scare you, just being real).
Breaking down everyday use, Prilosec’s sweet spot is gastroesophageal reflux disease, or GERD. People with GERD know it well: it’s that constant regurgitation, sour taste, and cough that refuses to leave. Prilosec calms the acid splash with daily use, letting your throat and esophagus heal. Doctors also rely on it for healing stomach ulcers and preventing new ones (especially if you take painkillers like ibuprofen, which can wreck your stomach lining).
But there are times Prilosec is not your friend. Not for instant symptom relief (Tums wins that round), and definitely not for pregnant women unless a doctor says so. There are also drug interactions to watch for. If you’re taking Plavix (clopidogrel) for your heart, Prilosec weakens it, raising your heart attack risk.
Let’s clear up a big myth: More is not better. People sometimes take double doses when symptoms flare, but that only raises your risk of side effects—without any extra gain. Stick to what’s recommended; your gut will thank you.
One more thing—it’s not just about popping a pill. Prilosec works best when it’s taken before a meal (usually breakfast), not after you’re already in pain. That’s because you want the drug in your system before your stomach starts pumping out acid. Mix it up, and you’ll miss out on full relief.
Check out these typical uses, as seen in real clinics:
| Condition | Typical Dose | Duration |
|---|---|---|
| GERD (adults) | 20 mg once daily | 4-8 weeks |
| Heartburn (OTC use) | 20 mg once daily | 14 days |
| Stomach Ulcer (H. pylori therapy) | 20-40 mg twice daily | 10-14 days |
And about that friend who swears by taking Prilosec every single day for years? They might want to chat with their doctor. Long-term use has hidden risks most people don’t realize—and you definitely don’t get a free pass just because it’s sold next to the vitamins.
Side Effects: What You Might Expect (and What to Watch For)
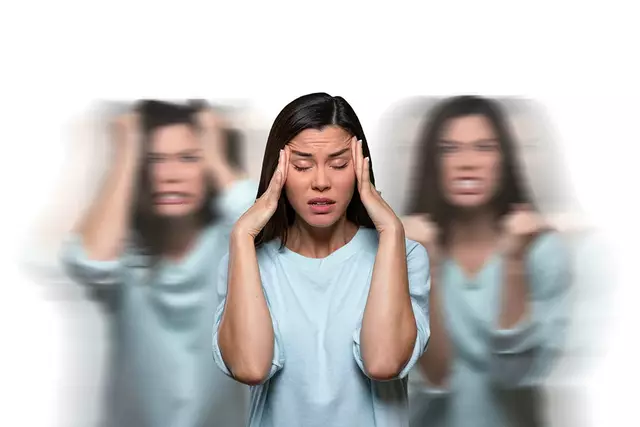
No pill is perfect, and Prilosec isn’t an exception. For most people, side effects are pretty mild, like a mild headache or a bit of nausea. But when used for months or even years, things can change. Your body needs stomach acid to absorb certain minerals and protect against infections, so blocking acid over the long haul brings a few surprises.
One big thing: low magnesium is a known risk. Your muscles and nerves need magnesium to fire correctly, and too little can lead to muscle cramps, trembling, irregular heartbeat, or even seizures. If you notice weird twitching or you’re feeling faint, it could be time to check your magnesium level, especially if you’re on Prilosec for weeks at a time.
Then there’s the issue of bones. Research published in "JAMA Internal Medicine" in 2023 found folks taking PPIs like omeprazole for over a year had a 25% higher risk of hip, wrist, and spine fractures. Your body needs acid to absorb calcium, and when that acid is gone, bones can get fragile. Not great news if you’re over 50, already at risk for osteoporosis, or don’t get much calcium in your diet.
Another strange twist: since stomach acid helps keep bacteria in check, less acid means more bacteria can survive. This increases the risk of gut infections, like Clostridioides difficile (C. diff), which leads to diarrhea that’s stubborn and sometimes severe. Hospitals keep close watch for C. diff in patients on Prilosec or other PPIs.
Sometimes, side effects are subtler. People complain about belly bloating, tummy pain, or just not feeling right. A rare issue involves kidney problems—in some folks, the kidneys get inflamed and start losing function, usually after months of use. That’s why kidney tests are a smart idea for anyone who needs long-term PPI therapy.
Here’s a quick table for the most common side effects:
| Side Effect | Frequency |
|---|---|
| Headache | 1-7% |
| Nausea | 1-4% |
| Diarrhea | 2-3% |
| Abdominal pain | 1-5% |
| Low magnesium (long-term) | Rare but serious |
| Bone fracture (long-term) | Increased risk |
| Kidney disease (long-term) | Rare but serious |
A Mayo Clinic gastroenterologist put it perfectly:
“Like any medication, PPIs such as omeprazole give the greatest benefit with the least risk when used at the lowest effective dose for the shortest necessary time.”
It sounds obvious, but check with your doctor if you’re planning to take Prilosec for longer than the box recommends. They might suggest switching to a different approach, lowering your dose, or running a few safety labs to be sure you’re not at risk for hidden side effects.
Smart Tips: Getting the Most Out of Prilosec
Want Prilosec to work better and safer? Tiny shifts in your habits can make a big difference. First up: timing. Take Prilosec first thing in the morning, before you eat. That gives it a head start on your acid pumps, silencing them before breakfast even begins.
Second, pair your meds with basic heartburn hacks. Avoid supersized meals, stay upright after eating, and try not to snack too close to bedtime. Fried foods, mint chocolate, citrus, coffee, and especially alcohol ramp up acid production—even the best PPI can struggle with a pizza binge.
If you take other medications, double-check for interactions. Blood thinners, HIV drugs, antifungals, and even some anti-anxiety pills can run into problems. Pharmacists love when you ask questions—don’t be shy about showing them your whole list of meds.
Another tip: don’t crush or chew the pill. Prilosec has a protective coating so the medicine survives your stomach and makes it to where it works. Breaking the pill throws off the timing and ruins how it’s absorbed.
A lot of people worry about so-called “rebound” heartburn after stopping Prilosec. This is real: your body speeds up acid production when the drug leaves your system, sometimes making your reflux feel worse for a few days. Don’t panic—this usually settles after a week or two. Tapering your dose or using an antacid during this window can blunt the rebound until your stomach balances back out.
- Set a recurring reminder so you never miss a dose—skipping throws off your acid control.
- If you miss one dose, just take the next as scheduled. Doubling up doesn’t make up for lost time.
- Label changes can sneak up on you. Generic and brand meds often look different, so double-check it’s omeprazole every time you refill.
- If you’re taking supplements, look for chewies or liquids—big calcium or magnesium tablets are harder to absorb with less acid.
- Get your vitamin B12 checked yearly if you’ve been on Prilosec more than a few months—low acid makes it harder to absorb.
Prilosec isn’t addictive, but it can make you feel like you “need” it if reflux bounces back each time you stop. Sometimes folks need their doctor’s help to find newer medications or different lifestyle tricks if nothing else is working.

When to See a Doctor (and What Else Might Be Going On)
If Prada handbags and avocado toast ruled Instagram in 2018, it feels like heartburn’s quietly ruling the medicine cabinet in 2025. The thing is, that chest burn isn’t always what it seems. Worsening symptoms after you start Prilosec, pain that shoots down your arm, black or bloody stools, persistent vomiting, or weight loss all deserve attention from your doctor. Even hiccups: if you’re hiccupping constantly, it can be a hidden sign of esophageal trouble.
Some conditions look like heartburn but actually aren’t. Gallstones cause burning, as does anxiety, hiatal hernia, or—scariest of all—heart issues. Don’t ignore your gut instinct; if Prilosec isn’t cutting it and symptoms get weird, get checked out.
Prilosec doesn’t mix well with certain medical situations:
- If you’re pregnant or breastfeeding—always ask first. Studies show occasional Prilosec use seems safe, but chronic use hasn’t been tested enough to be sure.
- History of liver disease? Your doctor may want to adjust your dose.
- Autoimmune disorders or recurrent infections? Prilosec might mess with how your immune system works, and there are other options out there.
Kids and teens? Don’t reach for Prilosec unless a pediatrician makes the call. Children absorb and clear medicines differently, and acid isn’t always the troublemaker in young stomachs.
Sometimes doctors will suggest a short course of Prilosec for a tough case, then try switching their patient to a gentler option, like an H2 blocker (think Zantac or Pepcid). They may also run endoscopy tests or recommend imaging if something seems off.
Don’t be embarrassed to bring all your heartburn questions. A good doctor’s visit can give you a game plan, lower your risk, and maybe—just maybe—help you ditch the daily pill routine for good.







Brenda Taylor July 17, 2025
So I've been on Prilosec for a bit now and honestly, it sometimes feels like a godsend. But hey, not saying everyone should just pop these willy-nilly lol :)
What really gets me is how many folks just ignore the side effects listed because they wanna feel better immediately. And that's so risky! I mean, if you think about it, there are probably people out there mixing meds that shouldn't be combined and not realizing the consequences.
Also, it's wild how the post mentions safety tips but doesn't emphasize enough how important it is to actually read those instructions to the letter. Not saying I'm perfect but sometimes yall gotta hold yourselves accountable and not just rely on the doc’s words.
Anyway, did anyone else catch if Prilosec can be taken long-term without issues? Cause I’ve heard mixed stories from friends and family. Share your take?
virginia sancho July 18, 2025
Hey all! Just jumping in because I've been working in health services for years and wanted to add some clarity here.
Prilosec, or omeprazole, as it’s technically called, is indeed quite effective for controlling gastric acid-related problems. But as the post hints, it’s crucial that users don’t self-prescribe it without knowing their full health picture.
Long-term use can lead to nutrient absorption issues like magnesium deficiency or even increased risk for certain infections, so it’s essential to get regular follow-ups with your healthcare provider. It’s not just about popping a pill and ignoring other lifestyle habits that could be causing the problem.
Also, keep in mind that the medication might interact with drugs like blood thinners or antiretrovirals. So if you’re on other meds, definitely speak to your pharmacist or doctor before starting Prilosec.
I'd recommend everyone considering it to look beyond just the immediate relief and plan for holistic digestive health!
Namit Kumar July 20, 2025
This post is quite informative, but I must say sometimes we forget to factor in local practices when considering medications like Prilosec.
In India, we often lean on traditional remedies for digestion before moving to pharmaceuticals, which can be both a blessing and a curse. However, it’s important to realize that while Prilosec offers potent relief, it should be used responsibly.
I appreciate the detailed explanation of side effects and the warnings. It’s one thing to take medication, another to misuse it and cause bigger health concerns later.
Using emoticons to communicate serious health information might not be appropriate, but I get why some want to keep the tone light :)
Anyone here tried combining lifestyle changes with Prilosec? Curious to know what worked best for you!
Sam Rail July 21, 2025
Not gonna lie, I’ve used Prilosec a couple times when my reflux got out of hand. It does work, but sometimes these meds feel like a lazy fix, you know?
If you only treat symptoms and don’t deal with the causes then you might just end up taking more meds down the line. It’s annoying, but changing diet or habits really helps more long-term than just popping a pill.
That said, the article does a good job breaking down what to watch for with side effects.
Just wished it talked a bit more about how to wean off safely or alternatives if you don’t want to rely on it forever.
Taryn Thompson July 22, 2025
Thank you for this detailed article. From a clinical perspective, Prilosec is a proton pump inhibitor that revolutionized management of acid-related disorders. However, its use must always be balanced against potential risks.
Patients should be counseled on proper administration timing — usually before meals — and warned not to exceed recommended doses.
Moreover, the emerging evidence about long-term use including risks like bone fractures, kidney damage, and infections cannot be ignored.
My advice: only use Prilosec under medical supervision and for the shortest duration necessary. Regular evaluation will ensure that it's still necessary rather than a default medicine to mask ongoing issues.
Overall, an excellent primer for patients to understand the drug better, but never take this as a replacement for direct doctor advice.
Lisa Lower July 23, 2025
Hey everyone, just chiming in with some tips for making Prilosec use more effective because, trust me, it’s not just about swallowing a pill.
First, timing really matters — take it about 30-60 minutes before eating so it can do its job before acid flare-up.
And remember, while it can rock your symptoms, it's still part of a bigger approach — don't slack on lifestyle tweaks like avoiding trigger foods or stress management!
Also, never double dose if you forget once, and avoid long-term use unless clearly recommended by your doc to prevent risk buildup.
Finally, if you’re feeling off or experiencing new symptoms, don’t ignore it and just keep taking it — get a check-up ASAP!
Health’s not something to take lightly, folks, even if meds seem like an easy fix.
Dana Sellers July 24, 2025
Honestly, I find it irritating how so many folks just pop these meds without thinking twice. Like, it’s your body, take care of it. You wanna feel better? Then fix your lifestyle, stop relying on a pill to save you all the time.
I bet half the people on Prilosec are just masking problems caused by their bad eating habits, or stress they refuse to handle.
Besides, those side effects? Huge deal! You ignore them at your own risk. And don’t get me started on how much doctors sometimes over prescribe instead of pushing healthier choices.
Seriously, if you really care about your health, ditch the quick fix mentality and put in actual work.
Yeah, sorry if I sound harsh, but that’s the truth.
Damon Farnham July 25, 2025
I appreciate the comprehensive breakdown in this article, but might I point out that the overuse of such medications sometimes stems from a wider cultural neglect of self-discipline and traditional remedies prevalent in my region. It reflects a broader societal reliance on quick pharmaceutical fixes rather than sustainable health practices.
While Prilosec is effective, I find that embracing natural methods of managing digestion — dietary regimes, yoga, and meditation — has profound benefits that cannot be overlooked. The pharmaceutical industry, though necessary in many respects, should not eclipse these time-tested traditions.
That said, I agree with the article that one must heed safety guidelines and professional advice carefully to minimize adverse effects and interactions.
Does anyone here incorporate such holistic methods alongside their medication?
Marsha Saminathan July 26, 2025
Oh wow this post really sparked a lot for me. I’ve personally wrestled with acid reflux for years and Prilosec has been a rollercoaster of relief and side effects.
It’s so important to view this med as part of a bigger lifestyle overhaul — not just a magic pill. I found that combining it with mindful eating, avoiding late-night meals, and stress-busting activities helped me more than just taking it alone.
Also, the emotional ups and downs when dealing with chronic conditions like this often go unspoken but are equally crucial to address.
So yeah, thanks for the great info, but let’s keep sharing real lived experiences too, because medicine isn’t one size fits all.
Kavita Jadhav July 27, 2025
I really appreciate the detailed breakdown here, especially about who should avoid Prilosec — that’s a point many often overlook.
As someone who sees a lot of patients struggling with digestive issues, I’ve learned that being mindful of the root causes often prevents long-term dependency on medications like these.
Also, important to watch for symptoms that don’t improve or worsen — sometimes what feels like just heartburn can be a signal of more serious conditions.
And yes, always recommend checking with a healthcare professional before starting or stopping meds.
Glad to see such an informative guide out there for people trying to navigate these choices.
Alexia Rozendo July 29, 2025
Oh great another post about meds that people are gonna treat like candy. Seriously, can we PLEASE stop making these drugs the hero of every stomach ache story?
Like, hello? Maybe try not eating a whole extra-large pizza at midnight instead of relying on a pill that’s basically telling your stomach to shut up.
I’m all for doctors and science but the world ain’t gonna end if you look at your food choices first.
Anyway, rant over, great write-up though, if only people actually read the safety tips and didn’t just google the name and self medicate.