When you walk down the street and suddenly your legs feel heavy, numb, or cramp up-so much that you have to stop and lean on a shopping cart just to catch your breath-it’s easy to assume it’s a circulation problem. But if bending forward or sitting down makes the pain vanish, you’re likely dealing with something else: neurogenic claudication. This isn’t just a vague discomfort. It’s a clear signal from your spine that something’s pressing on your nerves. And if you’re over 50, you’re not alone. Around 200,000 Americans experience this each year, and the numbers are rising as the population ages.
What Exactly Is Neurogenic Claudication?
Neurogenic claudication isn’t a disease on its own. It’s a symptom of lumbar spinal stenosis, which means the space around your spinal nerves in the lower back has narrowed. This narrowing usually happens slowly over time due to wear and tear: bone spurs, thickened ligaments, or slipped discs crowd the space where nerves travel. When you stand or walk, those nerves get squeezed. The result? Pain, tingling, or weakness in your buttocks, thighs, or calves. The key to spotting it? Position. Unlike vascular claudication-where poor blood flow causes leg pain that goes away with rest-neurogenic claudication only improves when you bend forward. That’s why so many people with this condition find relief by leaning on a shopping cart, pushing a walker, or sitting down. It’s called the “shopping cart sign,” and it shows up in 68% to 85% of confirmed cases. If you can walk 200 feet before your legs give out, but then push a cart and walk the whole store? That’s a textbook sign.How Doctors Tell It Apart From Vascular Claudication
Mixing up neurogenic and vascular claudication is one of the most common diagnostic errors. And it matters. Treating a nerve problem like a blood flow issue won’t help-and could delay real treatment. Here’s how they’re different:- Neurogenic: Pain starts when standing or walking, gets worse with spine extension (standing straight), and improves with bending forward. Numbness, tingling, or weakness often accompany the pain. Foot pulses are normal.
- Vascular: Pain comes from poor circulation. It feels like cramping, happens during activity, and goes away with rest-even if you’re still standing. You might have cold feet, weak pulses, or a history of smoking or heart disease.
Why Imaging Alone Can Mislead
You might think an MRI is the final answer. But here’s the catch: up to 67% of people over 60 show signs of spinal stenosis on an MRI-even if they have zero symptoms. That means you can have narrowing without pain, and pain without severe narrowing. Imaging shows structure. It doesn’t tell you if that structure is causing your symptoms. That’s why diagnosis relies on the story you tell. If your history matches the pattern-pain with walking, relief with bending-and your physical exam supports it, doctors will trust that more than a scan. A negative straight leg raise test, normal reflexes, and no muscle wasting (except possibly in the small muscles of the foot, like the extensor digitorum brevis) all help confirm it’s nerve-related, not something else.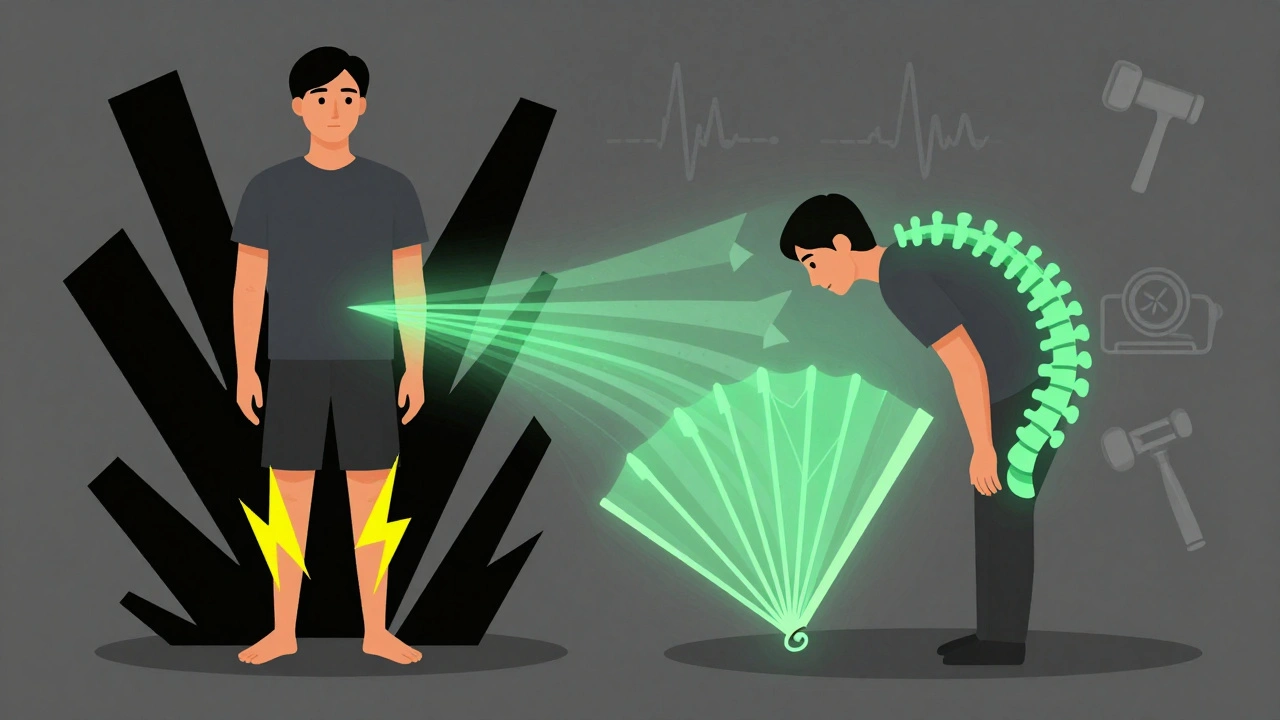
First-Line Treatment: Conservative Care
Most people don’t need surgery right away. In fact, 82% of early-stage patients see real improvement with conservative care. That means:- Exercise: Focus on flexion-based movements. Walking uphill, using a stationary bike with a forward lean, or doing pelvic tilts can help. Avoid exercises that arch your back.
- Physical therapy: A therapist will teach you posture techniques, core strengthening, and how to use your body to reduce pressure on the nerves. Six to eight weeks of consistent therapy is usually needed to see results.
- Pain management: Over-the-counter NSAIDs like ibuprofen can help with inflammation. For some, short-term muscle relaxants or nerve pain meds like gabapentin are used.
- Activity modification: Learn to use your environment. Carry a cane or walker. Lean on carts. Sit down when you can. These aren’t signs of weakness-they’re smart adaptations.
When Injections and Surgery Come Into Play
If conservative care doesn’t help after 3 to 6 months, and your pain is limiting your life, the next step might be an epidural steroid injection. These deliver anti-inflammatory medicine near the affected nerves. About half to 70% of patients get temporary relief-usually a few months. It’s not a cure, but it can buy time and reduce pain enough to get back into physical therapy. For those with persistent weakness, numbness, or pain that won’t quit, surgery is an option. The most common procedure is a laminectomy-removing part of the bone to open up space for the nerves. Minimally invasive versions are now common, with smaller incisions and faster recovery. A newer device called Superion, approved by the FDA in 2023, acts like a spacer between the bones in your lower back. In trials, 78% of patients were satisfied after two years. Success rates for surgery? Around 70% to 80% of well-selected patients report “good to excellent” improvement at one year. But surgery isn’t for everyone. If you’re not weak, and your pain is manageable with posture changes, you might never need it.
The Cost and the Future
Conservative treatment costs between $500 and $2,000 a year-mostly for therapy and meds. Surgery? That jumps to $15,000 to $50,000, depending on the hospital and procedure. Insurance usually covers it if it’s medically necessary, but out-of-pocket costs can still be steep. The big picture? Spinal stenosis is becoming more common. The global population over 65 will double by 2050. That means more people will face this condition. Research is moving toward better diagnostic tools-like a standardized algorithm being developed by the International Spine Study Group-to match symptoms with imaging more accurately. The goal isn’t just to treat pain, but to help people stay active longer.What to Do If You Think You Have It
If you’re over 50 and notice leg pain when walking that gets better when you bend forward:- Write down your symptoms: When does it start? What makes it better or worse?
- Try leaning forward while walking. Does it help? Keep track.
- See your doctor. Bring your notes. Ask: “Could this be neurogenic claudication?”
- Don’t accept a quick diagnosis of “poor circulation” unless your pulses are weak or you have other heart disease risk factors.
- Start with physical therapy. Don’t rush to surgery unless you’re losing strength or function.
Is neurogenic claudication the same as sciatica?
No. Sciatica is pain that radiates along the sciatic nerve, often from a herniated disc. It’s usually one-sided and sharp. Neurogenic claudication is caused by spinal stenosis and affects both legs or moves between them. It’s not a sharp pain-it’s heaviness, cramping, or numbness that builds up with walking and improves with forward bending.
Can I still walk if I have neurogenic claudication?
Yes, but you’ll need to adjust how you walk. Many people learn to walk in short bursts, then rest by leaning forward or sitting. Using a walker or shopping cart can extend your walking distance significantly. Regular, modified walking is actually part of treatment-it keeps muscles strong and improves nerve tolerance over time.
Why does bending forward relieve the pain?
Bending forward opens up the spinal canal. When you arch your back, the space narrows further and pinches the nerves. When you flex forward, the canal widens, taking pressure off the nerves. That’s why the “shopping cart sign” is so reliable-it’s a natural way your body finds relief.
Are there any exercises I should avoid?
Yes. Avoid exercises that extend your spine-like backbends, standing toe touches, or heavy lifting with a straight back. These increase pressure on the nerves. Instead, focus on seated or lying exercises that keep your spine in a neutral or flexed position: pelvic tilts, knee-to-chest stretches, and cycling with a forward lean.
What happens if I ignore it?
It usually gets worse slowly. You may notice you can walk shorter distances before pain hits. In rare cases, you could develop permanent weakness or loss of bladder/bowel control-this is a medical emergency called cauda equina syndrome. But most people don’t reach that point. The goal is to manage it early so it doesn’t limit your life.
Can weight loss help?
Yes. Extra weight puts more pressure on your spine, making stenosis symptoms worse. Losing even 5-10 pounds can reduce the load on your lower back and improve walking ability. Combine weight loss with core strengthening and it becomes a powerful tool for managing symptoms without surgery.





Louis Llaine December 6, 2025
So let me get this straight - if I lean on a shopping cart, I can walk through Target without turning into a human pretzel? And they call this medicine? 😏 I’ve been doing this since 2018 and thought I was just lazy. Turns out I’m just a genius with posture. Next thing you know, they’ll patent the shopping cart as a medical device and charge $2,000 for it.
Jane Quitain December 8, 2025
OMG this is so important!! I’ve been dealing with this for years and no one ever told me about the shopping cart trick!! 🥹 I started using my walker like a cane and now I can actually go to the grocery store without crying. You’re right - it’s not about being old, it’s about listening to your body. You’re a lifesaver!! 💪❤️
Ernie Blevins December 8, 2025
82% improve with PT? Lol. That’s just placebo with a clipboard. You think bending over fixes nerve compression? Nah. It’s the government’s way of keeping you docile. No one wants you to know the real cause: EMF from 5G towers is frying your spinal nerves. Look up the WHO’s suppressed 2018 study. They don’t want you walking. They want you sedentary. And now they’re selling you yoga mats and ibuprofen like it’s a solution. Wake up.
Nancy Carlsen December 9, 2025
Y’all this is so validating!! 🥲 I used to feel like a burden because I had to sit down every 5 minutes. Now I carry a tiny cushion in my purse so I can lean on benches like a pro 😅 And guess what? I started walking every day - just 10 minutes, leaning forward, smiling at strangers. My legs don’t feel like lead anymore. You’re not broken - you’re just adapting. And that’s brave. 💕
Jennifer Anderson December 10, 2025
i just found out i have this and i was like ohhhhh so thats why i always need to lean on the cart at walmart 😅 i thought i was just getting slow but turns out my spine is just being dramatic. physical therapy is kinda boring but i’m trying. also weight loss helped a little, not much but enough to make me feel less like a sack of potatoes. thanks for the info!!
Sadie Nastor December 11, 2025
Thank you for writing this. I’ve been scared to say anything because I didn’t want people to think I was just lazy. But now I realize - I’m not giving up, I’m adapting. I use a cane now, and I walk slower. But I’m still walking. That’s victory. 🌱 You’re right - this isn’t the end. It’s just a new way of moving through the world. I’m proud of myself for not quitting.
Nicholas Heer December 12, 2025
They’re hiding the truth again. Spinal stenosis? Nah. It’s the CDC’s secret bio-weapons program. They’ve been injecting fluoride into the water since 1948 to weaken our connective tissue. You think the VA is helping you? They’re just testing how long you’ll walk before you collapse. And that Superion device? Made by Lockheed Martin. You think they care about your pain? They care about your pension. Wake up. This is a control mechanism disguised as medicine.
Sangram Lavte December 13, 2025
I have a cousin in India who has this condition. He walks with a stick and leans on walls in markets. He never complained until he saw a video of someone using a walker. Now he says, ‘Ah, so this is what they mean by posture.’ He started physical therapy last month. Slow progress, but he smiles more now. This article helped him feel less alone. Thank you for sharing.