Introduction to Amiloride and Liver Function
As a blogger who's passionate about health and wellness, I always strive to provide my readers with the latest information on medical advancements and research. Today, I would like to discuss the impact of amiloride on liver function in patients with hepatic impairment. Amiloride is a medication primarily used to treat high blood pressure and fluid retention. However, its impact on liver function in patients with hepatic impairment has become an important topic of study in recent years.
Understanding Hepatic Impairment
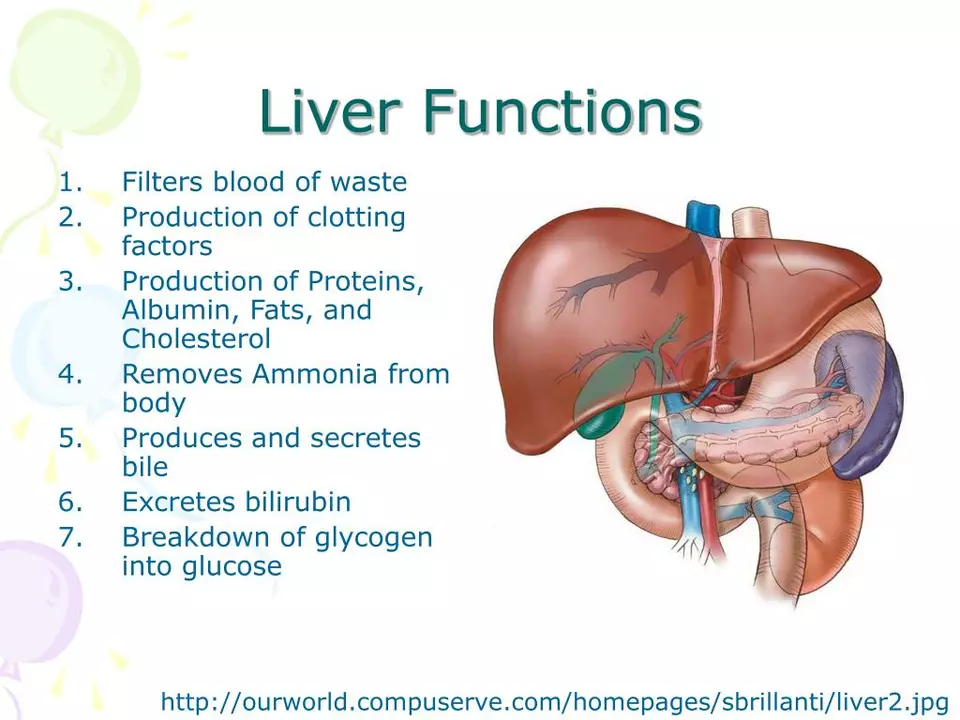
Before diving into the effects of amiloride, it's essential to understand what hepatic impairment is and why it's important. Hepatic impairment refers to the reduced function of the liver, which is responsible for detoxifying the body, processing nutrients, and producing essential proteins. This impairment can be caused by various factors, such as viral infections, excessive alcohol consumption, and chronic diseases like cirrhosis.
Patients with hepatic impairment often experience symptoms such as jaundice, fatigue, and swelling in the abdomen or legs. These symptoms can significantly impact a person's quality of life and, in severe cases, lead to life-threatening complications. Therefore, it's crucial to study the effects of medications like amiloride on liver function in this population.
Amiloride and Its Pharmacological Effects
Amiloride is a potassium-sparing diuretic medication that helps the body eliminate excess fluid and maintain a balanced level of electrolytes. It works by blocking the exchange of sodium and potassium in the kidneys, helping to reduce fluid retention and lower blood pressure. This medication is often prescribed in combination with other diuretics, like hydrochlorothiazide, to treat conditions such as congestive heart failure and hypertension.
As with any medication, it's essential to consider the possible side effects and interactions with other drugs. Some common side effects of amiloride include dizziness, headache, and gastrointestinal discomfort. However, the focus of this article is on the impact of amiloride on liver function in patients with hepatic impairment.
Research on Amiloride and Liver Function
Several studies have been conducted to understand the impact of amiloride on liver function in patients with hepatic impairment. These studies have focused on various aspects, including the metabolism of amiloride, its effect on liver enzymes, and the potential for liver toxicity.
One notable study found that the metabolism of amiloride is significantly altered in patients with hepatic impairment, leading to increased levels of the drug in the blood. This finding suggests that dosage adjustments may be necessary in this population to prevent potential side effects or toxicity. Another study found that amiloride could potentially increase the risk of liver toxicity in patients with pre-existing liver conditions, highlighting the importance of closely monitoring liver function in these patients.
Amiloride Dosage Adjustments for Hepatic Impairment
Given the potential impact of amiloride on liver function in patients with hepatic impairment, it's crucial to consider dosage adjustments to minimize the risk of side effects or toxicity. Some studies suggest that the dosage of amiloride should be reduced in patients with mild to moderate hepatic impairment, while others recommend close monitoring of liver function and electrolyte levels in these patients.
It's essential for healthcare providers to individualize the dosage based on each patient's specific needs and liver function. In some cases, alternative medications may be considered if the risk of amiloride-induced liver toxicity is deemed too high.
Monitoring Liver Function During Amiloride Treatment
For patients with hepatic impairment who are prescribed amiloride, regular monitoring of liver function is crucial to ensure the medication is not causing further damage to the liver. This monitoring may include periodic blood tests to measure liver enzyme levels, as well as assessments of overall liver function through imaging studies or other diagnostic tests.
In addition to liver function monitoring, healthcare providers should also carefully monitor electrolyte levels, kidney function, and blood pressure in patients with hepatic impairment taking amiloride. This comprehensive approach helps to minimize the risk of complications and optimize treatment outcomes.
Amiloride Contraindications and Precautions
While amiloride can be an effective treatment option for certain conditions, there are specific contraindications and precautions to consider, especially in patients with hepatic impairment. Amiloride is contraindicated in patients with severe hepatic impairment, as well as those with hyperkalemia (high potassium levels) or severe kidney disease.
In addition, healthcare providers should exercise caution when prescribing amiloride to patients with a history of liver disease or those taking medications known to impact liver function. Close monitoring and regular follow-up appointments are essential to ensure patient safety and the effectiveness of treatment.
Conclusion: The Importance of Personalized Treatment
In conclusion, the impact of amiloride on liver function in patients with hepatic impairment is a crucial consideration for healthcare providers and patients alike. While this medication can be an effective treatment option for conditions like hypertension and congestive heart failure, it's essential to individualize the dosage and closely monitor liver function in patients with compromised liver function.
By taking a personalized approach to treatment and considering each patient's unique needs, healthcare providers can minimize the risk of complications and help improve the quality of life for patients with hepatic impairment. As a blogger passionate about health and wellness, I hope that this article has provided valuable insights into the complex relationship between amiloride and liver function in this vulnerable population.






Sydnie Baker May 29, 2023
The pharmacokinetic intricacies of amiloride in the context of hepatic dysfunction merit rigorous scrutiny.
The recent hepatological literature underscores a non-linear augmentation of the drug's half-life concomitant with escalating Child–Pugh scores.
Such a phenomenon precipitates an elevated plasma concentration, thereby potentiating nephrotoxic sequelae and perturbations in electrolyte homeostasis.
Moreover, the inhibition of the epithelial sodium channel (ENaC) appears to be modulated not merely by renal expression but also by hepatic enzymatic variability.
Clinicians must therefore recalibrate dosing regimens, privileging a titration algorithm that integrates both hepatic and renal functional indices.
It is incumbent upon prescribers to requisition baseline liver function tests-namely alanine aminotransferase, aspartate aminotransferase, and bilirubin-prior to initiation.
Serial monitoring, ideally biweekly during the induction phase, facilitates the early detection of idiosyncratic hepatocellular injury.
In parallel, the concomitant administration of potassium-sparing diuretics mandates vigilant surveillance of serum potassium to preempt hyperkalemia.
The extant corpus of randomized controlled trials, albeit limited in sample size, consistently advocates for a 25–30% dose reduction in patients classified as Child–Pugh B.
For those occupying the Child–Pugh C stratum, the preponderance of evidence suggests outright contraindication.
Furthermore, pharmacogenomic considerations, such as polymorphisms in the CYP3A4 isoenzyme, may further refine individualized therapeutic strategies.
The interdisciplinary collaboration between hepatologists, nephrologists, and clinical pharmacologists is thus indispensable.
Patient education should emphasize the salience of reporting symptoms such as unexplained jaundice, pruritus, or abdominal discomfort.
In summation, the judicious use of amiloride amidst hepatic impairment epitomizes the quintessence of precision medicine.
By harmonizing dosage adjustments with meticulous laboratory oversight, clinicians can mitigate adverse outcomes while preserving therapeutic efficacy.
Ultimately, the confluence of empirical data and nuanced clinical judgment will dictate optimal patient‑centered care.
Benjie Gillam June 8, 2023
Philosophically speaking, the liver can be seen as the body's alchemical crucible, transmuting toxins into harmless metabolites.
When we perturb this delicate balance with amiloride, we are essentially challenging the very essence of homeostasis.
It's a reminder that every pharmacologic intervention carries an ontological weight that extends beyond mere symptom control.
Definately, clinicians should contemplate the broader metaphysical implications of dosing adjustments.
In practice, that means aligning the drug's kinetic profile with the patient's lived experience, not just their lab values.
Ultimately, this perspective fosters a more humane approach to therapeutic decision‑making.
Naresh Sehgal June 19, 2023
Listen up, anyone messing with amiloride in a compromised liver needs to step up their game; the stakes are high and the margin for error is razor‑thin.
You can't just toss a standard dose and hope for the best-your patients' livers are screaming for precision.
Adjust the dosage, monitor the enzymes, and stop being lazy about potassium levels.
This isn't a suggestion; it's a command from the front lines of clinical responsibility.
Prove you have the grit to fine‑tune therapy and save lives, not just write scripts.
Poppy Johnston June 29, 2023
Hey, I totally get the intensity-you’ve nailed the urgency, and that drive can really push the team to stay on top of monitoring.
Just remember to give yourself a breather too; the best care comes when we’re balanced and not burning out.
Johnny VonGriz July 9, 2023
I think we can all agree that tailoring amiloride doses for liver‑impaired patients is just good practice.
It’s not about over‑complicating things; it’s about being mindful of how the drug behaves in a different metabolic landscape.
Regular labs, clear communication with the patient, and a collaborative approach among specialists are the keys.
When everyone’s on the same page, adjustments become smoother and outcomes improve.
Real Strategy PR July 20, 2023
Your cavalier attitude toward dosing is downright unethical.
Doug Clayton July 30, 2023
Monitoring liver enzymes is essential but also keep an eye on electrolytes especially potassium levels they can swing quickly especially with amiloride
Michelle Zhao August 10, 2023
Indeed, the gravitas of prescribing a potassium‑sparing diuretic amidst hepatic derangement cannot be overstated; it is a veritable tightrope walk between therapeutic benefit and iatrogenic catastrophe.
One must wield the prescription pen with the solemnity of a surgeon brandishing a scalpel, ever cognizant of the latent perils that lurk beneath the surface of biochemical indices.
Eric Parsons August 20, 2023
From a philosophical standpoint, the principle of beneficence mandates that we harmonize pharmacological intervention with the physiological realities of hepatic insufficiency.
This alignment is not merely a procedural adjustment but a moral imperative to honor the intrinsic dignity of the patient’s bodily integrity.
Mary Magdalen August 31, 2023
Our nation's physicians should set the standard by pioneering meticulous dose‑modification protocols, showcasing that American medicine leads the world in safeguarding patients with compromised livers.
Dhakad rahul September 10, 2023
Behold, the saga of amiloride unfolds like an epic tale, where the heroic drug battles the villainous liver dysfunction-an odyssey worthy of legend! 😎
William Dizon September 20, 2023
Great analogy! It really helps visualize the challenge, and it reminds us to stay vigilant in our monitoring to ensure the “hero” doesn’t turn rogue.
Jenae Bauer October 1, 2023
Honestly, I bet there’s a big pharma plot behind all these dosage tweaks, trying to keep us guessing while they rake in profits from endless lab tests.
vijay sainath October 11, 2023
Typical corporate scheme-just another way to make you dependent on their meds and endless follow‑ups.
Daisy canales October 22, 2023
Wow thanks for the groundbreaking insight i had no idea that liver function matters when giving a diuretic
keyul prajapati November 1, 2023
It is worth noting that the longitudinal data from multicenter cohorts suggests a modest, yet statistically significant, correlation between elevated serum amiloride concentrations and incremental rises in transaminase levels among patients classified as Child–Pugh B; this observation, while not conclusive, does underscore the necessity for clinicians to consider both the pharmacodynamic profile of the agent and the underlying hepatic reserve when devising an individualized therapeutic regimen, thereby fostering an evidence‑based approach that balances efficacy with safety.
Alice L November 12, 2023
In accordance with the principles of cross‑cultural medical ethics, it is incumbent upon healthcare providers to integrate culturally sensitive counseling when discussing amiloride therapy with patients of diverse backgrounds, ensuring that knowledge of hepatic impairment and its implications is conveyed with respect, clarity, and reverence for the patient's cultural context.