Generic drugs make up 90% of all prescriptions filled in the U.S., but they only cost 10% of what brand-name drugs do. That sounds like a win for patients - and it is. But behind those low prices is a broken system. Many generic drug manufacturers are losing money. Some are barely breaking even. Others are shutting down production entirely. And when that happens, essential medicines disappear from shelves. This isn’t just a business problem. It’s a public health crisis.
The Price Collapse That No One Saw Coming
Ten years ago, a simple generic pill like amoxicillin might have sold for $0.50 per unit. Today, it’s $0.03. That’s not inflation. That’s a race to the bottom. When a brand-name drug loses its patent, dozens of manufacturers jump in. They all make the same thing. The only way to win is to undercut everyone else. And that’s exactly what they do. The result? Gross margins have collapsed from 50-60% in the early 2000s to under 30% today. For some products, they’re below 10%. Teva, once the world’s largest generic drugmaker, posted a -4.6% profit margin in 2025. That’s a $174 million loss on $3.8 billion in sales. Meanwhile, Mylan - now part of Viatris - managed a modest 4.3% margin. Why the difference? It’s not luck. It’s strategy.Three Paths to Survival
Generic manufacturers today aren’t all the same. They’re splitting into three distinct groups - and only two of them have a future. The first group still plays the old game: making simple, off-patent pills like metformin or lisinopril. Thousands of companies do this. The market is flooded. Profit margins are razor-thin. And every time a new player enters, prices drop again. This model is dying. In fact, the U.S. generic drug market shrank by 6.1% over five years through 2025. Companies that stick with this are just waiting to be bought - or shut down. The second group is moving into complex generics. These aren’t your everyday pills. They’re drugs that are hard to copy. Think inhalers with precise dosing, injectables with unstable ingredients, or combination pills with multiple active drugs. The FDA requires more testing. Fewer companies can make them. That means less competition - and higher prices. Lenalidomide, a cancer drug made as a generic by Teva, now sells for 10 times the price of a basic antibiotic. Why? Because only five companies can produce it reliably. That’s the new game. The third group? They don’t make drugs at all. They make them for others. These are contract manufacturing organizations (CMOs). Companies like Egis Pharmaceuticals launched their own CMO arms in 2023. They take raw ingredients and turn them into finished products for brand-name companies or other generics makers. This segment is growing at nearly 10% a year - from $51.96 billion in 2024 to $90.95 billion by 2030. Why? Because even big pharma companies don’t want to run their own factories anymore. Too expensive. Too risky. So they outsource.Why It’s Harder Than Ever to Start Up
You might think, “If the market is so big, why aren’t more companies jumping in?” Because the barriers are brutal. Getting FDA approval for a single generic drug costs about $2.6 million. That’s just the application fee. Then you need a manufacturing facility that meets current Good Manufacturing Practices (cGMP). Building one? At least $100 million. And that’s before you even start making pills. You need chemists, engineers, quality control teams, supply chain experts. And you need to prove you can do it consistently - month after month, year after year. Most new entrants fail. McKinsey found that over 65% of companies focusing only on simple generics don’t survive past two years. Why? They run out of cash before they get their first formulary placement. Hospitals and pharmacies won’t buy from a new supplier unless they’re sure the product won’t fail. And no one wants to be the first to test an unknown maker.
The Hidden Costs of Cheap Drugs
The savings from generic drugs are massive. In 2022 alone, they saved the U.S. healthcare system $408 billion. But those savings don’t go to the manufacturers. They go to insurers, PBMs (pharmacy benefit managers), and patients. Meanwhile, manufacturers are left with shrinking revenues and rising costs. Raw materials - like active pharmaceutical ingredients (APIs) - are often sourced from India or China. Prices swing wildly. A single shipment delay can shut down production. And when a drug goes on shortage - like insulin or chemotherapy agents - it’s often because no one can make it profitably anymore. Harvard’s Dr. Aaron Kesselheim put it bluntly: “The relentless price competition in generics has created a market failure where essential medicines face shortages because manufacturers cannot profitably produce them.”Who’s Winning - and How
Teva didn’t survive by making more amoxicillin. They pivoted. In 2024, they spent $998 million on R&D - up 5% - to develop complex generics and biosimilars. Their revenue grew 4% to $16.5 billion. Their profit came from drugs like Austedo XR, a treatment for movement disorders that only three companies can produce. Viatris took a different path. After merging Mylan and Upjohn in 2020, they sold off their biosimilars unit, their OTC business, and their API division. Why? To focus on what they do best: distributing established generics at scale. They cut costs, streamlined operations, and focused on markets where pricing is less brutal - like parts of Europe and Latin America. In 2024, they grew revenue by 2% - not because they sold more pills, but because they stopped losing money on the wrong ones. And then there’s the contract manufacturing boom. Companies like Catalent, Lonza, and now Egis Pharma Services are stepping in to fill the gap. They don’t need to own the brand. They just need to make the product. And they get paid regardless of who sells it.
The Global Picture
The U.S. market is the most competitive - and the most broken. But elsewhere, things look different. In Europe, governments set prices based on value, not just cost. That means manufacturers can charge more for complex generics. In India and China, low labor costs and strong domestic demand make it easier to stay profitable. Emerging markets like Brazil and Indonesia are seeing double-digit growth in generic use - but they come with risks: currency swings, regulatory delays, and corruption. The global generic market is projected to hit $600 billion by 2033. But that growth won’t come from the U.S. It’ll come from complex drugs, biosimilars, and contract manufacturing - especially in Asia and Latin America.What’s Next?
The next five years will decide which generic manufacturers survive - and which become footnotes. If you’re still making simple pills, you’re on borrowed time. The market is saturated. Margins are gone. The only way out is to sell - or pivot. If you’re building complex generics, you’re in the right place. But you need deep technical expertise, strong regulatory teams, and a willingness to invest in R&D. You can’t compete on price. You compete on skill. If you’re a contract manufacturer, you’re in the sweet spot. Demand is rising. Barriers to entry are lower. And you don’t have to worry about who owns the brand. Just make it right - and get paid. The truth is, generic drugs aren’t going away. They’re too important. But the business model that made them cheap is dead. The new model isn’t about making more pills. It’s about making better ones - and making them for people who can’t make them themselves. The patients still need their medicines. The question is: who will be left to make them?Why are generic drug prices falling so fast?
When a brand-name drug’s patent expires, dozens of manufacturers start making the same generic version. Since the drugs are identical, the only way to win customers is to offer the lowest price. This creates a race to the bottom. Over time, prices drop until manufacturers can barely cover production costs - sometimes even below them. This is especially true in the U.S., where pharmacy benefit managers (PBMs) negotiate bulk discounts that squeeze manufacturers’ margins.
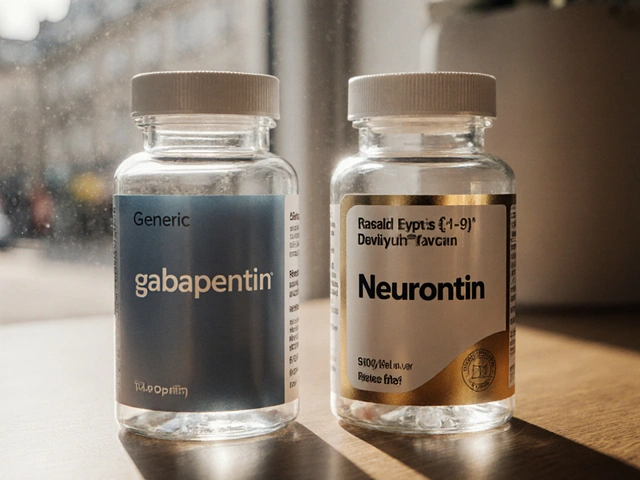
What are complex generics, and why are they more profitable?
Complex generics are drugs that are hard to copy because of their formulation, delivery method, or ingredients. Examples include inhalers, injectables, and combination pills with multiple active drugs. Making them requires advanced technology, strict quality control, and extensive testing. Fewer companies can produce them, so competition is lower. That lets manufacturers charge higher prices - sometimes 5 to 10 times more than simple generics - while still being cheaper than the original brand.
Why do generic drug shortages happen?
Shortages occur when manufacturers stop producing a drug because they can’t make money on it. A simple generic like amlodipine might cost pennies to make, but if the selling price drops below $0.01 per pill, it’s not worth the cost of compliance, labor, or shipping. When multiple manufacturers quit making the same drug, supply chains break. The FDA tracks these shortages, but there’s no quick fix - because the root cause is economic, not technical.
Can contract manufacturing save the generic industry?
Yes - in part. Contract manufacturing organizations (CMOs) don’t compete on drug prices. They compete on reliability, speed, and technical expertise. They make drugs for brand-name companies, generic makers, and even startups. This model is growing fast because it removes the risk of owning a brand while still generating steady revenue. Companies like Egis and Catalent are expanding rapidly, and this segment is expected to reach $91 billion by 2030. But CMOs alone can’t replace the lost volume of commodity generics.
Are generic drug profits going to recover?
Not for the old model. Simple, low-cost generics will keep losing money. But the future lies in complex generics, biosimilars, and contract manufacturing. The next wave of patent expirations - including blockbuster drugs for diabetes, heart disease, and cancer - will create new opportunities. Companies that invest in technical capability and regulatory expertise will thrive. Those that don’t will disappear.






Asha Jijen November 27, 2025
generic drugs are just a scam now. everyone gets ripped off except the big pharma middlemen. why do we even bother?
Edward Batchelder November 28, 2025
This is an incredibly important discussion, and I appreciate how thoroughly you've laid out the systemic issues. The collapse of margins isn't just an economic problem-it's a moral one. We've optimized for cost at the expense of sustainability, and now we're paying for it with access to life-saving medications. We need policy intervention, not just market fixes.
reshmi mahi November 29, 2025
india makes 70% of the world's generics and still we're getting crushed?? 😂😂😂
laura lauraa November 30, 2025
The commodification of human health has reached its logical, grotesque conclusion. When a pill for hypertension is sold for three cents, and the person who synthesized it cannot afford rent, we have entered a post-ethical society. This is not capitalism. This is necro-economics.
Gayle Jenkins December 2, 2025
I love how this post breaks down the three paths forward. It's not doom and gloom-it's strategy. If you're still making amoxicillin, it's time to pivot. But if you're building complex generics or CMOs? You're not just surviving-you're building the future of healthcare. This is the kind of insight that changes industries.
Kaleigh Scroger December 3, 2025
The real issue is that the FDA approval process is designed for brand-name drugs not generics and the cost structure doesn't scale down even though the product complexity does which means even if you're making a complex generic you're still spending 2.6 million just to get approval and then you need a cGMP facility that costs 100 million and that's before you even start testing stability or bioequivalence and by then the market has already been flooded by someone who cut corners and sold cheaper and now you're bankrupt and the whole system is rigged against innovation because the only thing that matters is price per pill and not quality or reliability or patient outcomes and honestly we're all just waiting for the next insulin shortage to happen again
Elizabeth Choi December 4, 2025
Teva's -4.6% margin is a red flag, but the real story is that their R&D spend increased 5% while revenue only grew 4%. That's not innovation-it's desperation. They're throwing money at a sinking ship.
Allison Turner December 6, 2025
everyone thinks they're smart until they realize the only people making money are the ones who don't make pills at all
Darrel Smith December 7, 2025
This is what happens when you let corporations run healthcare! They don't care about people-they care about profit margins! They'd rather let people die than raise a single penny on a pill! It's evil! It's immoral! And the government is letting it happen because they're in the pocket of PBMs and big pharma! We need a revolution!
Aishwarya Sivaraj December 9, 2025
i think what people miss is that when you make a generic you dont just make a pill you make trust and when that trust breaks because of quality issues or shortages it takes years to rebuild and india and china arent just cheap theyre scalable and if we want to bring production back we need to invest in training and not just factories and honestly we need to stop pretending this is just about price its about dignity
Iives Perl December 10, 2025
CMOs are a front. The government owns them. You think they let private companies make life-saving drugs? Nah. It's all a cover for the shadow pharma cartel. 🤫💊
Alex Hess December 11, 2025
The fact that anyone still believes this is a free market is laughable. You call this capitalism? It's a cartel rigged by regulators and PBMs to crush small players. The only winners are the ones who never made a single pill.
Jonah Thunderbolt December 11, 2025
The real villain isn't Teva or Mylan-it's the FDA. They're the gatekeepers who turned a simple process into a $100 million obstacle course. And don't get me started on how they approve biosimilars faster than generics. It's all about who you know. 🤡
Rebecca Price December 12, 2025
I find it deeply concerning that we've normalized the idea that essential medicines should be priced at the lowest possible level, regardless of the human cost. This isn't a business model-it's a public health failure. We must recalibrate our values.
marie HUREL December 13, 2025
I think the CMO model is actually the most promising. It takes the pressure off companies to own the brand and lets them focus on what they do best-making high-quality products. It’s a quiet revolution, but it’s happening. I hope more people notice.