Mycosis Fungoides Intimacy Impact Checker
Impact Analysis Results
Finding out you have Mycosis Fungoides is a rare type of cutaneous T‑cell lymphoma that manifests as skin patches, plaques, or tumors can feel like a punch to the gut. The diagnosis doesn’t just bring medical appointments; it shakes up the everyday rhythms you share with a partner. From itchy lesions that make a simple cuddle uncomfortable to the anxiety of being seen as ‘different’, the disease can quietly erode intimacy and strain relationships. Below you’ll discover why it happens and, more importantly, what you can do right now to keep the connection strong.
Key Takeaways
- Physical symptoms such as itching, pain, and visible lesions directly impact touch and sexual activity.
- Emotional reactions-shame, fear, and altered body image-often create a hidden barrier between partners.
- Open, factual communication about symptoms and treatment side‑effects reduces misunderstandings.
- Tailoring intimacy to comfort levels, using lubrication, moisturizers, and positioning, can preserve sexual pleasure.
- Professional help-from dermatologists, counselors, and support groups-offers practical tools for coping.
Understanding Mycosis Fungoides and Its Physical Footprint
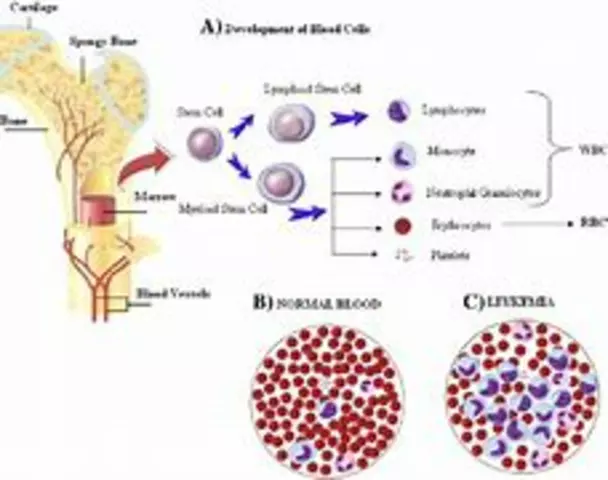
The disease belongs to the broader family of Cutaneous T‑Cell Lymphoma (CTCL). While it usually starts as flat, scaly patches on the torso or limbs, it can progress to raised plaques or tumor‑like nodules. Common physical issues that intersect with intimacy include:
- Persistent itching: scratching can cause skin breaks, making touch painful.
- Dry, cracked skin: lesions often lack natural moisture, leading to discomfort during hugging or intercourse.
- Painful inflammation: flare‑ups can be tender, limiting certain positions.
- Visible changes: discoloration or thickened patches may affect body confidence.
Even if the disease is medically stable, these daily sensations become a silent partner in the bedroom, dictating when and how affection is expressed.
Emotional and Psychological Ripples
Beyond the skin, Mycosis Fungoides triggers a cascade of emotions. A 2023 patient‑survey from the International Mycosis Fungoides Association reported that 68% of respondents felt a dip in self‑esteem within three months of diagnosis. The mental load often looks like:
- Body image concerns: noticing new spots or scars can make a person withdraw from physical closeness.
- Fear of rejection: worries that a partner will find the lesions unattractive or contagious.
- Stress about future health: uncertainty about disease progression can cloud present‑moment enjoyment.
- Isolation: feeling that no one else truly gets the daily discomfort.
When these feelings pile up, intimacy may shift from physical to emotional, and a couple can lose the balance they previously enjoyed.

Partner Communication: The First Line of Defense
Clear, compassionate dialogue is the fastest way to stop misconceptions from fester. Here’s a quick script you can adapt:
- State the facts: “I have Mycosis Fungoides, a skin lymphoma that causes itchy patches.”
- Share the impact: “Sometimes the itching makes hugging uncomfortable, and certain positions hurt.”
- Invite questions: “What worries you most about this?”
- Offer solutions: “I’ve found moisturizers and specific positions that help; let’s try them together.”
- Set a check‑in: “Can we talk about how this feels for both of us after each week?”
Listening without judgment and acknowledging your partner’s feelings fosters a team mindset, turning a medical challenge into a shared problem to solve.
Practical Tips for Maintaining Physical Intimacy
Even with flare‑ups, couples can keep the spark alive. Below are actions that work for most patients:
- Moisturize before contact: apply a fragrance‑free, urea‑based cream to lesions 15 minutes before hugging to reduce friction.
- Use hypoallergenic lubricants: during sexual activity, silicone‑based lubricants prevent additional irritation.
- Adjust lighting and temperature: warm rooms and soft lighting help relax muscles and lower itch intensity.
- Explore non‑penetrative intimacy: massage, kissing, or using a vibrator can provide pleasure without stressing affected skin.
- Choose positions that avoid pressure: side‑lying or seated positions reduce contact with painful patches.
These small changes often make the difference between a painful encounter and a pleasurable one.
How Common Treatments Influence Intimacy
| Treatment | Typical Side‑Effects Relevant to Intimacy | Mitigation Strategies |
|---|---|---|
| Phototherapy | Skin dryness, temporary redness | Intensive moisturizing, schedule sessions on low‑intimacy days |
| Systemic Therapy (e.g., interferon, oral retinoids) | Fatigue, mood swings, decreased libido | Plan intimate moments for higher‑energy periods, discuss mood changes with a therapist |
| Topical Steroids | Skin thinning, burning sensation | Apply as prescribed, use barrier creams before sexual activity |
Understanding which side‑effects are likely lets you pre‑empt discomfort and keep the bedroom schedule realistic.

Support Networks: From Body Image to Counseling
When a diagnosis feels isolating, reaching out to groups that "get it" can lift the emotional load. You might consider:
- Support Groups: online forums or local meet‑ups for Mycosis Fungoides patients often share skin‑care hacks and coping stories.
- Relationship Counseling: a therapist trained in chronic illness can guide couples through communication pitfalls.
- Body Image Workshops: programs that use mindfulness and acceptance techniques to rebuild confidence.
Even a single session can provide a fresh perspective, making it easier to discuss intimate topics without shame.
Checklist for Couples Managing Mycosis Fungoides
- Schedule a joint doctor’s visit to discuss treatment side‑effects on intimacy.
- Pick a moisturiser and lubricants that are fragrance‑free and test them on a small skin area first.
- Set a weekly “talk‑time” to share feelings about skin changes and sexual needs.
- Identify two non‑penetrative activities that both partners enjoy.
- Join at least one support group or online community within the next month.
- Consider a short‑term counseling session if communication stalls.
Crossing each item off can turn anxiety into action, reinforcing that you’re tackling the disease together.
Next Steps and Troubleshooting
If you notice any of the following, act quickly:
- Increasing pain during contact: consult your dermatologist about adjusting treatment dosage.
- Sudden drop in desire: a mental‑health professional can explore depression or medication side‑effects.
- Partner feels detached: revisit communication guidelines and perhaps schedule a couples’ therapy session.
Remember, the goal isn’t to return to a pre‑diagnosis “normal” but to create a new rhythm that respects both health and love.
Frequently Asked Questions
Can Mycosis Fungoides be passed to a partner through sexual contact?
No. Mycosis Fungoides is a type of lymphoma that originates from your own immune cells. It isn’t contagious, so physical intimacy won’t spread the disease.
What if my lesions appear on my genitals?
Genital involvement is less common but can happen. Use a water‑based, fragrance‑free lubricant, and keep the area clean and moisturized. Speak with your dermatologist about gentle topical options that won’t irritate during sex.
How often should I talk to my partner about my symptoms?
Aim for a brief check‑in at least once a week, plus a deeper conversation when a flare‑up begins or when treatment changes. Consistency builds trust.
Do treatments like phototherapy affect my sexual drive?
Phototherapy mainly causes skin dryness and temporary redness-effects that are manageable with moisturisers. It rarely influences libido directly, unlike some systemic drugs that may cause fatigue or mood changes.
Is it normal to feel ashamed of my skin?
Yes, many patients report body‑image concerns. Processing those feelings with a therapist or a support group can help you rebuild confidence and reduce the shame barrier.
Living with Mycosis Fungoides doesn’t have to mean saying goodbye to closeness. By tackling the physical symptoms, opening honest dialogue, and leaning on professional help, couples can rediscover intimacy on their own terms.







Alex EL Shaar October 9, 2025
Honestly, most people read a glossy article on Mycosis Fungoides and think it's just another skin hassle, but the reality is a gnarly cocktail of itch, pain, and self‑esteem demolition. The constant scratching is like a tiny saboteur carving trenches into your epidermis, turning every hug into a battlefield. If you’re not using a urea‑rich cream, you’re basically inviting a flare‑up fiesta. And don’t even get me started on those “non‑contagious” reassurances – they feel like a stale band‑aid on a bleeding wound. Partners who act like it’s a minor inconvenience are basically drinking the poison while you’re suffering. Communication is the only shield that isn’t a placebo, so drop the vague “I’m fine” and spell out the damn triggers. Bottom line: treat the skin, treat the psyche, or you’ll watch intimacy dissolve faster than a sugar cube in tea.
Anna Frerker October 16, 2025
Freedom of love should not be shackled by a rare lymphoma; the body’s rebellion is a personal war, not a political statement.
Julius Smith October 24, 2025
Looks like you’ve got a whole manual for bedroom gymnastics, lol 😂
Brittaney Phelps October 31, 2025
Great list! Try the side‑lying position tonight and see if the pressure eases. You’ll thank yourself tomorrow.
Kim Nguyệt Lệ November 7, 2025
It is important to note that moisturizers containing ceramides have been shown in clinical studies to reduce transepidermal water loss, thereby decreasing itch intensity during intimate moments. Additionally, the use of a hypoallergenic silicone‑based lubricant can prevent friction without compromising skin barrier function. Monitoring skin response after each session and documenting any aggravation can provide valuable data for your dermatologist to adjust treatment protocols.
Rhonda Adams November 14, 2025
Hey, you’re absolutely right about the need for open dialogue! 🌟 I always tell couples to set a “comfort check‑in” before any intimate activity – just a quick, honest question like “How’s your skin feeling right now?” can save a lot of awkwardness later. Pair that with a good moisturizer routine (think fragrance‑free, hyaluronic acid) and you’ll notice a big drop in irritation. And don’t forget to celebrate the small wins; a gentle hug that doesn’t trigger a flare is a victory worth a high‑five! 🙌 Keep the conversation flowing and the love will find its way through the skin.
Macy-Lynn Lytsman Piernbaum November 21, 2025
Life throws us curveballs like stubborn skin lesions, but intimacy is still a canvas we can paint with patience and humor. 🌱 The mind’s narrative often amplifies the itch, turning a simple touch into an existential dread. If we reframe the experience as a shared adventure rather than a medical obstacle, the emotional weight lightens. Think of each moisturizer application as a ritual of care, each conversation as a bridge across the unknown. In the end, it’s the willingness to stay present that turns the tide.
Alexandre Baril November 28, 2025
Thanks for the tip! I’ve started using a fragrance‑free cream after showers and it’s already lessening the itch during cuddles.
Stephen Davis December 6, 2025
That’s awesome, Alex! 🌈 It’s amazing how a tiny change in the bedtime routine can feel like you just unlocked a secret level in the game of love. Keep experimenting with those gentle positions and you’ll find the sweet spot where comfort meets connection.
Grant Wesgate December 13, 2025
Totally agree, Stephen. 😎 Sometimes the simplest tweaks-like a softer pillow or dimmed lights-make the whole experience feel like a spa night for two.
Richard Phelan December 20, 2025
Hold on a second-are we really suggesting that a handful of moisturizers can single‑handedly resurrect a dying romance? The tragedy of Mycosis Fungoides is not some melodramatic soap opera where a love potion fixes the plot. It’s a relentless saga of skin betrayal, emotional turbulence, and the desperate clutch for intimacy amidst the storm. Yet, I must commend the relentless optimism; it’s the kind of fierce hope that fuels the fire of perseverance. Let’s not sugar‑coat the struggle, but let’s also not drown in despair-balance is the true hero here.
benjamin malizu December 27, 2025
From a pathophysiological standpoint, the epidermal barrier dysfunction inherent in CTCL precipitates a cascade of neurogenic inflammation, which, when compounded by psychogenic stressors, exacerbates dyspareunia. Therapeutic modulation via topical calcineurin inhibitors, in conjunction with psychosexual counseling, can mitigate the nociceptive feedback loop. Moreover, integrating a biopsychosocial model ensures that both somatic and affective dimensions are addressed in a cohesive treatment algorithm.
Maureen Hoffmann January 3, 2026
I’ve seen countless couples navigate the rough waters of Mycosis Fungoides and come out stronger on the other side.
The first step is always to acknowledge that the disease is a partner, not a villain.
When you share a vulnerable moment, you’re actually building a bridge of trust.
Start each day with a brief check‑in: a simple question like “How does your skin feel this morning?” can set the tone.
Pair that with a ritual-apply a fragrance‑free emollient together, massaging it in slow, calming strokes.
The physical act of caring for each other's skin reinforces emotional intimacy.
If flare‑ups occur, remember that they are temporary signals, not permanent roadblocks.
Communicate openly about what sensations are tolerable and which positions need adjustment.
Experiment with pillows, blankets, and ambient lighting to create a soothing environment that distracts from discomfort.
Incorporate non‑penetrative pleasures such as gentle massage, cuddling, or shared meditation to keep the connection alive.
Don’t shy away from professional help; a therapist specializing in chronic illness can provide tools to navigate emotional turbulence.
Similarly, a dermatologist who understands the psychosocial impact can tailor treatments that minimize itching during intimate moments.
Celebrate small victories-a night without scratching, a lingering kiss, a comfortable hug-and let those moments fuel your confidence.
Remember that intimacy is a spectrum; it isn’t limited to sexual activity alone.
By broadening the definition of closeness, you relieve pressure on the body and nurture the heart.
Stay patient, stay compassionate, and you’ll discover that love can thrive even in the presence of a chronic condition.