For millions of people around the world, stomach pain, bloating, and erratic bowel habits aren’t just inconvenient-they’re life-limiting. If you’ve been told your symptoms are "just stress" or "all in your head," you’re not alone. But here’s the truth: irritable bowel syndrome isn’t a psychological disorder. It’s a real, measurable breakdown in communication between your gut and your brain.
What Is IBS, Really?
Irritable bowel syndrome (IBS) affects between 5% and 10% of people globally. It’s not an infection. It’s not cancer. It’s not something you can see on a scan. But it’s also not imaginary. The Rome IV criteria, used by doctors worldwide since 2016, define IBS by three key patterns: recurrent abdominal pain at least one day a week for three months, linked to bowel movements, and tied to changes in stool frequency or form. That’s it. No inflammation. No structural damage. Just a misfiring system. Yet, nearly 8 out of 10 people with IBS report non-painful discomfort-pressure, fullness, or aching-that doesn’t fit the textbook definition. Over half also struggle with anxiety or depression. And here’s the twist: it’s not that stress causes IBS. It’s that the gut and brain are stuck in a feedback loop where each one amplifies the other’s signals.The Gut-Brain Axis: Your Body’s Hidden Wiring
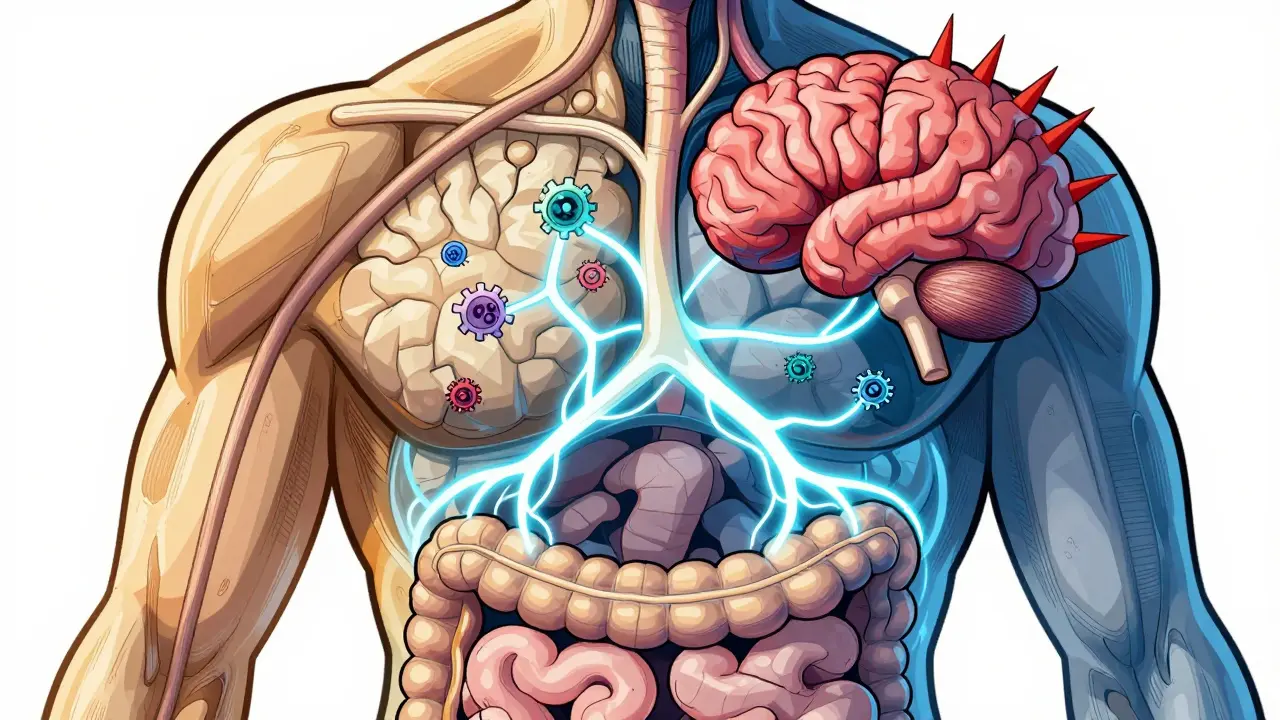
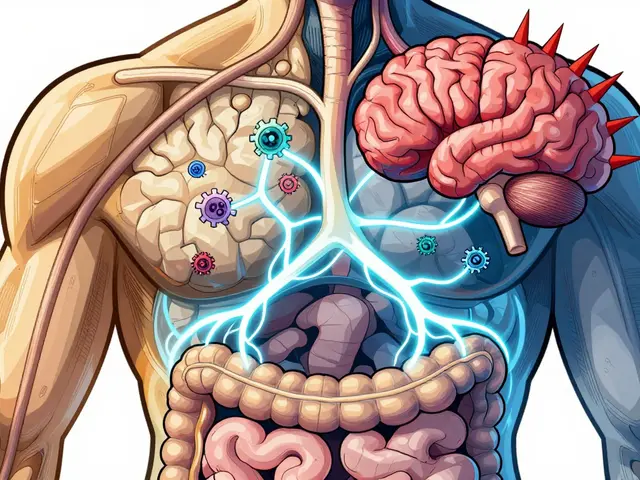
Think of your gut as a second brain. It’s lined with over 100 million nerve cells-the enteric nervous system-that operate independently, controlling digestion, blood flow, and immune responses. These nerves talk directly to your central nervous system through the vagus nerve, the body’s longest cranial nerve. Hormones, immune signals, and even the trillions of microbes in your intestines all send messages back and forth. In people with IBS, this system is out of sync. Brain scans show clear differences: the hypothalamus, which handles stress and gut control, is overactive. The prefrontal cortex, which helps regulate emotions and pain, is underactive. In diarrhea-predominant IBS (IBS-D), the brain areas that process body sensations are thicker. In constipation-predominant IBS (IBS-C), the regions that sense internal discomfort are thinner. These aren’t random changes. They’re biological signatures of a system that’s lost its balance. Serotonin, the same chemical linked to mood, is mostly made in your gut-95% of it. In IBS-D, levels spike, speeding up digestion and triggering diarrhea. In IBS-C, serotonin drops, slowing everything down. Immune cells in the gut also produce less natural painkillers like β-endorphin, making you more sensitive to even normal gut movements. It’s not that your gut is broken. It’s that your brain is interpreting normal signals as dangerous.Why Diets Like Low-FODMAP Work (and Why They’re Hard)
The low-FODMAP diet is one of the most effective tools for IBS relief, helping 50-76% of people in clinical trials. FODMAPs are short-chain carbohydrates found in foods like onions, garlic, wheat, apples, and dairy. They’re poorly absorbed in the small intestine, drawing water into the gut and fermenting rapidly in the colon. That fermentation produces gas, stretches the bowel, and triggers pain signals in a hypersensitive system. But the diet isn’t simple. It involves a strict 4-6 week elimination phase, followed by careful reintroduction. Many people give up because it’s confusing, restrictive, and socially isolating. And it’s not a cure-it’s a management tool. The goal isn’t to avoid FODMAPs forever, but to find your personal tolerance level. Working with a registered dietitian who understands IBS is critical. Without guidance, you risk nutrient deficiencies and unnecessary food fear.
Gut-Directed Hypnotherapy: The Silent Game-Changer
If you’ve ever heard of hypnotherapy for IBS and thought it sounded like pseudoscience, you’re not alone. But here’s what the science says: in randomized trials, gut-directed hypnotherapy leads to symptom improvement in 70-80% of patients. That’s better than most medications. And the effects last-6 months later, most people still feel better. How does it work? It doesn’t make you sleepwalk or cluck like a chicken. It trains your brain to reinterpret gut signals. Through guided relaxation and imagery, patients learn to calm the nervous system’s overreaction to normal digestion. One patient described it as “rewiring my alarm system.” Unlike drugs that mask symptoms, hypnotherapy changes how your brain processes pain. It’s not magic. It’s neuroplasticity. The catch? Access is limited. Certification requires over 100 hours of training and 20 supervised cases. In rural areas, there’s often just one certified practitioner per 500,000 people. And out-of-pocket costs can run $1,200-$2,500 for a full course. Insurance rarely covers it. But for those who’ve tried everything else, it’s often the turning point.Probiotics, FMT, and the Microbiome Mystery
Your gut is home to trillions of microbes-bacteria, fungi, viruses. In IBS, the balance is off. Studies show lower diversity and shifts in key groups like Firmicutes and Bacteroidetes. Some probiotics help. Bifidobacterium infantis 35624, taken daily at one billion colony-forming units, improved global symptoms in 30-40% of users compared to placebo. That’s modest, but meaningful for people with no other options. Fecal microbiota transplantation (FMT)-transferring stool from a healthy donor-is more dramatic. Response rates vary wildly: 20% to 60%. Why? Because we still don’t know which microbes matter most, or how to standardize the process. The FDA treats FMT as a biological product, not a therapy, and requires strict donor screening. It’s promising, but not yet ready for routine use.Medications: Targeting the Axis, Not Just Symptoms
Traditional IBS meds-antispasmodics, laxatives, anti-diarrheals-often fail because they don’t touch the root cause. Newer drugs do. For IBS-D, alosetron blocks serotonin receptors in the gut, slowing transit. It’s FDA-approved for women with severe symptoms, but carries a risk of serious intestinal complications. Prucalopride, a serotonin agonist, helps IBS-C by stimulating contractions. Both work because they speak the same language as the gut-brain axis. But drugs aren’t perfect. Side effects are common. In one survey, 63% of IBS patients quit medications within three months due to nausea, headaches, or fatigue. That’s why experts now recommend a stepped approach: education first, diet second, then targeted meds or neuromodulation for those who need more.
The Future: Biomarkers, Personalization, and Hope
The biggest breakthrough in 2023 was the launch of VisceralSense™, a blood test that measures 12 microbial metabolites and neurotransmitter ratios to predict how someone will respond to treatment-with 85% accuracy. Imagine knowing before you start a diet or drug whether it’s likely to work for you. That’s personalization, not guesswork. The NIH’s $15 million Microbiome-Gut-Brain Consortium and the EU’s Gut-Brain Atlas Project are mapping this system in unprecedented detail. We’re moving from treating symptoms to fixing the communication network. By 2030, experts predict gut-brain axis therapies will make up nearly half the IBS market, replacing outdated, one-size-fits-all approaches.What You Can Do Today
You don’t need to wait for the future to feel better. Start here:- Learn the gut-brain connection. Understanding that your pain is real, biological, and reversible reduces shame and increases treatment adherence.
- See a dietitian trained in low-FODMAP. Don’t go it alone.
- Explore gut-directed hypnotherapy. Look for practitioners certified by the American Society of Clinical Hypnosis.
- Track your symptoms. Note food, stress, sleep, and bowel patterns. Patterns reveal triggers.
- Ask your doctor about serotonin-targeting meds if other options fail. Don’t settle for ineffective treatments.
Why This Matters
IBS isn’t just about your bowels. It’s about how your entire body responds to stress, food, and environment. When you stop seeing it as a gut problem and start seeing it as a brain-gut-microbiome system failure, you unlock real solutions. You’re not broken. Your wiring is just noisy. And with the right approach, you can turn down the volume.Is IBS the same as IBD?
No. IBS (irritable bowel syndrome) is a functional disorder-your gut looks normal on scans but doesn’t work right. IBD (inflammatory bowel disease), which includes Crohn’s disease and ulcerative colitis, involves visible inflammation, ulcers, and tissue damage. IBD requires different treatments, often immunosuppressants or biologics. IBS doesn’t cause cancer or permanent damage.
Can stress cause IBS?
Stress doesn’t cause IBS, but it can trigger or worsen symptoms. People with IBS have a more reactive gut-brain axis. Stress activates the HPA axis, which sends signals to the gut that alter motility, secretion, and pain sensitivity. That’s why anxiety often coincides with flare-ups. Managing stress isn’t optional-it’s part of treatment.
Are probiotics worth trying for IBS?
Some strains work, but not all. Bifidobacterium infantis 35624 has the strongest evidence, showing 30-40% improvement over placebo. Other strains like Lactobacillus plantarum 299v and certain multi-strain blends also show benefit. Avoid generic probiotics labeled only as "for digestive health"-they’re not backed by IBS-specific trials. Look for products that list the exact strain and CFU count.
How long does it take for low-FODMAP diet to work?
Most people notice improvement within 2-6 weeks on the elimination phase. Some feel better in just a few days. But the diet isn’t meant to be permanent. After symptoms improve, you slowly reintroduce FODMAPs one group at a time to find your personal tolerance. This phase is crucial-cutting out too many foods long-term can harm your gut microbiome.
Is IBS more common in women?
Yes. Women are two to three times more likely to be diagnosed with IBS. Hormones play a role-estrogen and progesterone affect gut motility and pain sensitivity. Many women notice worse symptoms around their period. But IBS affects men too, and they’re often underdiagnosed because they’re less likely to seek help. Gender doesn’t change the underlying mechanism-it just changes how symptoms present.
Can IBS be cured?
There’s no known cure, but many people achieve long-term remission. With the right combination of diet, stress management, and targeted therapies, symptoms can become mild or disappear for months or years. The goal isn’t to eliminate IBS forever-it’s to regain control so it doesn’t control you.
What’s the best way to find a good gut-directed hypnotherapist?
Look for practitioners certified by the American Society of Clinical Hypnosis (ASCH) or the British Society of Clinical and Academic Hypnosis (BSCAH). Ask if they have specific training in gut-directed hypnotherapy for IBS-not general hypnosis. Many offer virtual sessions, which increases access. Check reviews from other IBS patients and ask about their success rates.






Chris Urdilas January 27, 2026
So let me get this straight - we’ve got a whole system wired like a bad Wi-Fi connection, and the solution is to pay $2,500 for someone to whisper nice things to your colon? I’m sold. Also, why does every IBS article sound like a TED Talk written by a pharmaceutical rep who just discovered the word 'neuroplasticity'?
Jeffrey Carroll January 29, 2026
This is one of the most scientifically grounded and compassionate overviews of IBS I’ve encountered. The emphasis on the gut-brain axis as a bidirectional communication network, rather than a psychological issue, aligns with current neurogastroenterology research. The inclusion of evidence-based interventions - from low-FODMAP protocols to gut-directed hypnotherapy - provides actionable pathways for patients who have been dismissed for too long. Well done.
Phil Davis January 30, 2026
70-80% success rate with hypnotherapy? That’s more than my last relationship. And yet, somehow, it’s still considered ‘alternative.’ Meanwhile, my doctor gave me a pill that made me feel like a zombie and told me to ‘just chill.’ Thanks, medicine.
Irebami Soyinka January 30, 2026
USA always think they own the science 😒 Nigeria has had natural gut healers for centuries - ginger, bitter leaf, uziza seeds. You pay $2500 for hypnosis? We chant and drink herbs and feel better in 3 days. This is why Africa still has wisdom while you all pay for ‘biohacks’ that your grandmas knew for free. 🌿😂
Kevin Kennett February 1, 2026
Look, I’ve been there - the bloating, the panic before leaving the house, the shame of needing to find a bathroom every 20 minutes. I tried everything: gluten-free, dairy-free, keto, even acupuncture. Nothing worked until I found a gut-directed hypnotherapist. It didn’t feel like magic. It felt like my brain finally stopped screaming at my gut. If you’ve tried meds and diets and still feel broken - give this a shot. You’re not crazy. Your nerves are just overworked.
Jess Bevis February 1, 2026
Low-FODMAP works. But don’t quit carbs forever. Reintroduce slowly. Your microbiome will thank you.
Rose Palmer February 3, 2026
It is imperative to underscore that the clinical efficacy of gut-directed hypnotherapy, as substantiated by randomized controlled trials, represents a paradigm shift in the management of functional gastrointestinal disorders. Furthermore, the integration of biomarker-driven personalization, exemplified by VisceralSense™, heralds a new era of precision medicine in gastroenterology. Patients are strongly advised to consult with licensed practitioners and registered dietitians prior to initiating any therapeutic protocol.
Kathy Scaman February 5, 2026
Just tried the low-FODMAP diet. Lasted 3 days. Ate a bowl of onion soup. Regretted nothing. Still have IBS. Still happy. 🤷♀️