Weight‑Loss Drug Choice Quiz
Alli (Orlistat) is an over‑the‑counter lipase inhibitor that blocks about 30% of dietary fat absorption. Approved by the U.S. Food and Drug Administration, each softgel delivers 60mg of Orlistat and is taken with meals containing fat.
Why people reach for Alli
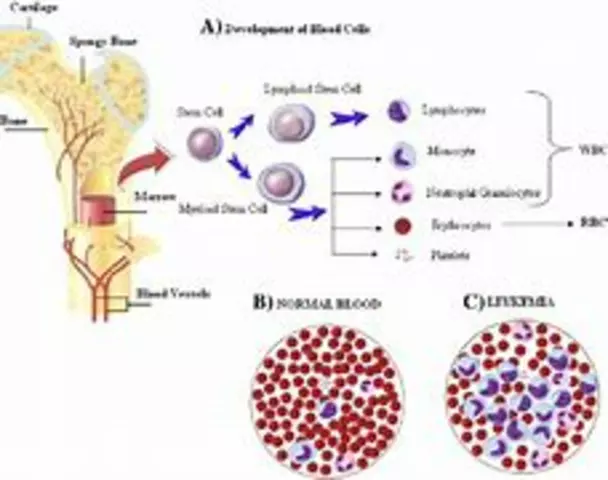
Alli targets the digestive step where dietary fat is broken down by pancreatic lipase. By attaching to the enzyme’s active site, it prevents the enzyme from cleaving triglycerides into absorbable free fatty acids. The undigested fat is then excreted, which can lead to a modest weight loss of 3-5% of body weight after 12 weeks when paired with a low‑fat diet.
Key attributes of Alli:
- Dosage: 60mg per meal (up to three times daily)
- OTC availability: Yes, in pharmacies and supermarkets
- Typical users: Adults with a BMI≥25kg/m² (or≥23kg/m² with obesity‑related risk factors)
- Common side effects: Oily spotting, flatulence, urgent bowel movements
Who should consider Alli?
Ideal candidates are people who can commit to a diet where less than 30% of calories come from fat. If you have gallbladder disease, chronic malabsorption, or are on a cyclosporine, Orlistat may be contraindicated. A short course of a multivitamin (especially vitamins A, D, E, K) is often advised because the drug reduces fat‑soluble vitamin absorption.
Major alternatives on the market
Weight‑loss pharmacotherapy isn’t limited to Orlistat. Below are the most common prescription and OTC options that people compare against Alli.
Xenical is the prescription‑strength version of Orlistat (120mg). It follows the same mechanism but is usually reserved for patients needing a stronger effect. Phentermine is an appetite suppressant classified as a sympathomimetic amine. It stimulates norepinephrine release, reducing hunger signals. Contrave combines bupropion (an antidepressant) with naltrexone (an opioid antagonist). The duo works on the hypothalamic reward pathway to curb cravings. Qsymia merges phentermine with topiramate, a seizure medication that also promotes satiety and increases energy expenditure.OTC supplements such as Garcinia cambogia, green‑tea extract, or raspberry ketone are also marketed for weight loss, but they lack robust clinical data and are not FDA‑approved for this indication.
Side‑effect profile comparison
Understanding side effects helps you decide which agent aligns with your tolerance and health status.
| Drug | FDA status | Mechanism | Typical dosage | Avg. weight loss (12weeks) | Main side effects |
|---|---|---|---|---|---|
| Alli (Orlistat) | OTC | Lipase inhibition (fat malabsorption) | 60mg ×3 meals | 3-5% | Oily spotting, GI urgency, vitamin deficiency |
| Xenical (Orlistat) | Prescription | Same as Alli, 120mg | 120mg ×3 meals | 5-7% | Similar GI issues, higher risk of liver enzymes elevation |
| Phentermine | Prescription | Appetite suppressant (sympathomimetic) | 15-37.5mg daily | 5-10% | Increased heart rate, insomnia, dry mouth |
| Contrave (bupropion/naltrexone) | Prescription | Reward‑pathway modulation | 8mg/90mg BID (titrated) | 5-9% | Nausea, dizziness, possible mood changes |
| Qsymia (phentermine/topiramate) | Prescription | Combined appetite suppression + satiety | 3.75/23mg → 15/92mg daily (titrated) | 7-10% | Paraesthesia, cognitive slowing, elevated heart rate |

How to decide which option fits you
Think of the decision as a three‑step filter:
- Medical suitability: Do you have conditions that rule out stimulant‑based drugs (e.g., hypertension, heart disease) or malabsorption issues that make Orlistat risky?
- Lifestyle match: Are you comfortable eating a low‑fat diet and taking a multivitamin (Alli) or would you prefer a pill that works without changing food composition (Phentermine, Qsymia)?
- Risk tolerance: GI side effects versus cardiovascular or neuro‑psychiatric effects - weigh which side‑effect profile you can live with.
For many, starting with the least invasive option-Alli-makes sense because it’s OTC, has a well‑documented safety record, and doesn’t affect heart rate or blood pressure. If after 12 weeks the weight loss is insufficient and you have no contraindications, moving to a prescription drug under a doctor’s supervision is the logical next step.
Practical tips for getting the most out of Alli
- Stick to meals with ≤30% calories from fat; this minimizes oily stools.
- Take the capsule with a full glass of water at the start of the meal-not after.
- Supplement vitamins A, D, E, K at least 2hours apart from the dose.
- Track progress weekly; a 0.5-1kg loss per week signals effectiveness.
- Stay hydrated and consider a fiber‑rich diet to soften stools.
Related concepts that influence weight‑loss drug choice
Understanding the broader health picture helps you talk intelligently with your clinician.
Body Mass Index (BMI) measures weight relative to height (kg/m²) and is the primary eligibility criterion for most pharmacologic interventions.A low‑fat diet is essential for Orlistat efficacy because the drug works only on ingested fat. Typical recommendations limit dietary fat to 20-30g per meal.
When fat absorption drops, vitamin supplementation becomes necessary to avoid deficiencies in fat‑soluble vitamins (A, D, E, K).
Patients on stimulant‑type drugs (Phentermine, Qsymia) should have baseline blood pressure and heart rate assessments, as these agents can raise both metrics.
Finally, a comprehensive lifestyle modification plan-including regular exercise, sleep hygiene, and stress management-amplifies any pharmacologic benefit.
If you’re leaning toward Alli, order a pack from a reputable pharmacy, schedule a quick consult with your GP to confirm no contraindications, and set up a 12‑week tracking sheet. If you suspect a prescription drug might suit you better, book an appointment with a weight‑management specialist and bring this comparison table as a conversation starter. Yes, but separate them by at least two hours. Since Orlistat blocks fat absorption, the vitamins need a fat‑based carrier to enter the bloodstream. Alli contains 60mg of Orlistat per capsule and is sold OTC. Xenical is the prescription version with 120mg per dose, intended for patients needing a stronger fat‑blocking effect. No. The FDA advises against using Orlistat during pregnancy or lactation because reduced fat absorption could affect fetal development and infant nutrition. Reduce dietary fat for that meal, stay hydrated, and wear protective undergarments if needed. The symptom usually lessens as your body adjusts. Combining two weight‑loss agents is generally discouraged unless a specialist explicitly recommends it. Overlapping side‑effects, especially gastrointestinal ones, can become problematic. Most guidelines suggest a trial of 12-24 weeks. If you achieve at least 5% body‑weight loss and tolerate the drug, you may continue under medical supervision. Orlistat can reduce the absorption of cyclosporine, levothyroxine, and warfarin. Always inform your pharmacist and doctor about all medications and supplements you take.Next steps for readers
Frequently Asked Questions
Can I take Alli and a multivitamin at the same time?
How does Alli differ from Xenical?
Is it safe to use Alli while pregnant or breastfeeding?
What should I do if I experience oily spotting?
Can I combine Alli with prescription weight‑loss drugs?
How long should I stay on Alli?
Are there any food or drug interactions I should know about?






Adele Joablife September 25, 2025
When you look at Alli’s mechanism, you realize it’s a very niche tool – it only works if you’re willing to overhaul your diet, which eliminates a large chunk of potential users. The fat‑blocking effect is solid, but the gastrointestinal side‑effects are a real deterrent for many. If you can't commit to a low‑fat regimen, the drug basically becomes a placebo. Meanwhile, the prescription versions add modestly more potency for a price hike that many aren’t ready to justify. In short, Alli is best suited for disciplined dieters who can tolerate the messy side‑effects, not for the casual “quick‑fix” crowd.
kenneth strachan September 29, 2025
i think orlistat is like, totally overrated lol.
Mandy Mehalko October 3, 2025
Hey folks! I totally get the hesitation around those oily side‑effects – they sound gross, but remember that with a consistent low‑fat diet you can actually keep them in check. If you keep a food diary and stay under the 30% fat threshold, most people report that the stool issues fade after a few weeks. Keep your spirits up, every tiny step counts toward that 5% goal!
Bryan Kopp October 7, 2025
While some people are busy picking pills, we should remember that a strong, home‑cooked meal is the real patriotic act – it builds the nation from the gut up. If you’re not willing to choose wholesome foods, no drug will save you from the inevitable health decline.
Patrick Vande Ven October 11, 2025
Alli (Orlistat) operates via inhibition of pancreatic lipase, an enzyme essential for hydrolyzing dietary triglycerides into absorbable free fatty acids. By binding irreversibly to the active site of this enzyme, the drug reduces the hydrolysis of approximately 30% of ingested fat, which subsequently passes unaltered through the gastrointestinal tract and is expelled in the feces. This pharmacodynamic action mandates a concomitant reduction in dietary fat intake, typically to less than 30% of total caloric consumption, to mitigate the frequency and severity of adverse gastrointestinal events such as oily spotting, flatulence, and urgency. The necessity for accompanying supplementation with fat‑soluble vitamins A, D, E, and K arises from the drug’s propensity to diminish their absorption, thereby posing a risk for deficiency states if unaddressed. Clinical trials have demonstrated a modest average weight reduction of 3‑5% of initial body weight after a 12‑week treatment course, contingent upon adherence to both the low‑fat diet and the medication regimen. Comparative efficacy data reveal that higher‑dose prescription Orlistat (Xenical) yields a slightly superior weight loss outcome, approximately 5‑7%, owing to the doubled drug exposure per meal. However, the side‑effect profile remains largely consistent across both formulations, with no substantial increase in severe adverse events reported. In contrast, sympathomimetic agents such as Phentermine and Qsymia produce more pronounced weight loss (5‑10%) but introduce cardiovascular concerns, including tachycardia, hypertension, and potential arrhythmias, necessitating rigorous cardiac monitoring. Bupropion/naltrexone (Contrave) and topiramate‑containing regimens similarly achieve greater weight reductions but carry neuropsychiatric and cognitive side‑effects, respectively, which may limit their suitability for certain populations. The decision algorithm for clinicians should therefore prioritize patient‑specific factors: comorbid hypertension, cardiac disease, gallbladder pathology, pregnancy status, and tolerance for gastrointestinal discomfort. For patients with contraindications to stimulant‑type agents or who prefer a non‑systemic mode of action, Alli remains a viable first‑line therapy, provided they are willing to integrate lifestyle modifications and vitamin supplementation. Ultimately, the therapeutic hierarchy aligns as follows: initial trial of Alli for low‑risk individuals, escalation to prescription Orlistat for enhanced efficacy, and progression to appetite‑suppressant or combinatorial agents for refractory cases, all under vigilant clinical supervision.
Tim Giles October 15, 2025
Considering the pharmacokinetic profile of Orlistat, one might wonder about the impact of variable gastric emptying times on its efficacy. If a patient consistently consumes meals with delayed gastric emptying, could the drug’s window of activity be compromised, leading to reduced fat absorption inhibition? Moreover, does the concomitant intake of fiber‑rich foods, which can alter the viscosity of intestinal contents, enhance or impede the drug’s mechanism? It would be valuable to examine whether timing the multivitamin supplementation at least two hours apart from the Orlistat dose consistently restores fat‑soluble vitamin levels across heterogeneous patient populations. Finally, given the modest weight‑loss percentages observed, how does the cost‑effectiveness ratio compare to that of newer GLP‑1 receptor agonists, which, albeit injectable, demonstrate higher average weight reductions? A systematic review addressing these nuances would greatly aid clinicians in tailoring therapy.
Peter Jones October 19, 2025
I think the best approach is to match the drug to the patient’s lifestyle and medical history. If someone can stick to a low‑fat diet, Alli is a low‑risk option. If rapid results are needed and there are no cardiovascular issues, a prescription appetite suppressant might be appropriate.
Gerard Parker October 23, 2025
From a practical standpoint, the first thing anyone should do before picking a weight‑loss drug is to talk to a qualified clinician. They’ll run basic labs, check blood pressure, and assess any gallbladder or malabsorption concerns. If you qualify for Alli, make sure you stock up on a good quality multivitamin-without it you’ll be shortchanging vitamins A, D, E, and K. And remember: consistency beats intensity. Take the pill with every meal that contains fat, keep your diet under 30% fat, and you’ll see steady results without the jittery side‑effects of stimulant‑based drugs.
Thomas Burke October 27, 2025
Hey all, just a quick heads‑up: if you decide to try Alli, stay hydrated and consider adding extra fiber to keep things moving smoothly. Also, pair the pill with a low‑fat snack if you feel any urgency-helps the stomach settle.
Debbie Frapp October 31, 2025
Can anyone share how they track their daily fat intake while on Alli? I’m using a phone app, but I’m curious if there are any tricks to stay under that 30% threshold without feeling deprived.
Michelle Abbott November 4, 2025
From a mechanistic viewpoint, the lipase inhibition caused by Orlistat is a classic example of competitive enzymatic blockade, yet the clinical translation is hampered by patient non‑adherence to dietary fat limits. The resultant fecal lipid excretion-while theoretically advantageous for caloric deficit-introduces a cascade of malabsorption‑related sequelae that are often under‑reported in trial data. Moreover, the necessity of concurrent vitamin supplementation adds a layer of complexity that can diminish patient compliance, especially in populations with limited health literacy. In summary, the drug’s pharmacological elegance is undermined by its real‑world practicality.
Heather Jackson November 8, 2025
Wow, the whole low‑fat diet thing is like, a total nightmare for anyone who loves pizza. I tried it for a week and my life felt like a bad drama series-no cheese, no joy. Honestly, if you can’t live without pizza, maybe this isn’t the right path for you.
Akshay Pure November 12, 2025
One must approach the discussion of Orlistat with the intellectual rigor it deserves; the drug represents a marginal advancement in pharmacotherapy, yet the marketing hype inflates its significance beyond evidence‑based parameters. The necessity of a strict dietary regimen, coupled with the inconvenience of vitamin supplementation, renders it an impractical choice for the discerning patient. A more nuanced, literature‑driven appraisal would suggest reserving its use for highly compliant individuals, not the average consumer.
Steven Macy November 16, 2025
Reflecting on the broader implications, it’s clear that weight‑loss medication should be viewed as a complement-not a substitute-to holistic lifestyle change. Ethical prescribing involves ensuring patients understand both benefits and burdens, fostering shared decision‑making, and supporting sustainable habits beyond the pharmacologic window.
Matt Stone November 20, 2025
Alli helps you lose weight it’s cheap and easy
Joy Luca November 24, 2025
When you evaluate the risk‑benefit profile of Orlistat, the gastrointestinal side‑effects are a non‑trivial consideration that can significantly impact adherence, especially in patients unaccustomed to a low‑fat diet regimen, and thus any recommendation must be personalized to the individual's metabolic tolerance and lifestyle constraints.
jana caylor November 28, 2025
The grammar in the article is solid, but watch out for the occasional typo in the dosage instructions; clear communication is key when patients are self‑medicating.
Vijendra Malhotra December 2, 2025
From a cultural perspective, it’s important to recognize that dietary habits vary worldwide; providing region‑specific guidance on low‑fat meals can improve adherence and outcomes for diverse patient populations.
Nilesh Barandwal December 7, 2025
Indeed, the discussion surrounding Orlistat’s efficacy is multi‑faceted; one must consider not only the pharmacological mechanism but also the sociocultural context in which patients operate, thereby ensuring that therapeutic recommendations are both scientifically sound and culturally resonant!;
Elise Smit December 11, 2025
Great summary! Remember to keep the multivitamin at least two hours apart from the dose and stay consistent with the low‑fat diet for best results.