When you pick up a prescription, you might not notice the difference between the brand-name pill and the generic one sitting in your bag. But behind that switch is a detailed, science-backed system called Therapeutic Equivalence Codes-or TE codes. These aren’t just labels. They’re the reason your pharmacist can legally swap your expensive brand-name drug for a cheaper generic without asking your doctor. And they’re why millions of Americans save billions every year without sacrificing safety or effectiveness.
What Are TE Codes, Really?
Therapeutic Equivalence Codes are a rating system created by the U.S. Food and Drug Administration (FDA) to tell pharmacists and doctors which generic drugs can be safely swapped for brand-name versions. Think of them like a green light for substitution. If a generic drug has an "A" code, it means the FDA has tested it and confirmed it works just like the brand-name drug-same active ingredient, same dose, same way it’s absorbed by your body, and same clinical effect.
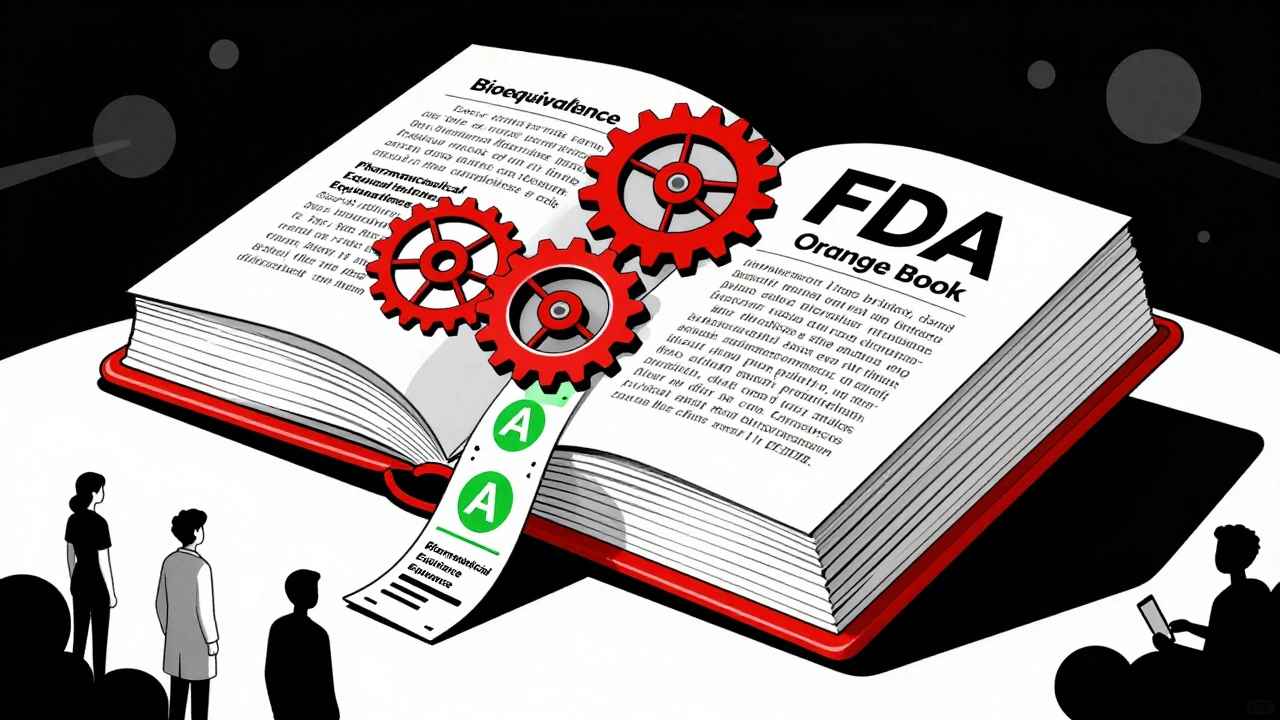
The system lives in the FDA’s Orange Book, officially called Approved Drug Products with Therapeutic Equivalence Evaluations. It’s updated every month, and every generic drug approved since 1984 gets a TE code. The first letter tells you the big picture: "A" means therapeutically equivalent. "B" means it’s not. Simple.
But it gets more specific. The second letter tells you the type of product. "AA" means it’s a powder you mix into a liquid, like some antibiotics. "AN" is for injectable solutions. "AT" is for topical creams. These details matter because a cream that looks the same might not deliver the drug the same way if the base ingredients are different.
How Does the FDA Decide a Generic Is Equivalent?
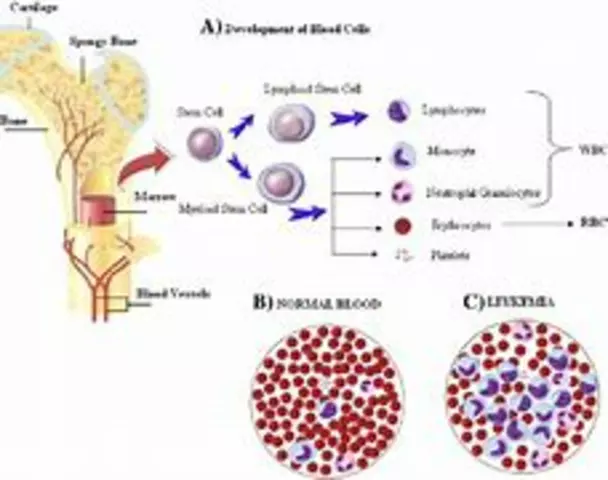
The FDA doesn’t just take a generic manufacturer’s word for it. To get an "A" rating, the drug must pass three strict tests:
- Pharmaceutical equivalence: The generic must have the exact same active ingredient, strength, dosage form, and route of administration as the brand. No exceptions. If the brand is a 10mg tablet taken by mouth, the generic must be identical.
- Bioequivalence: This is the real test. The generic must release the drug into your bloodstream at the same rate and to the same extent as the brand. The FDA requires studies showing that the amount of drug absorbed (called AUC) and the peak level in your blood (called Cmax) fall within 80% to 125% of the brand’s numbers. That’s a tight window-tight enough to catch even small differences in how the pill breaks down.
- Clinical equivalence: The drug must work the same way in the body. For most drugs, bioequivalence proves this. But for tricky ones-like blood thinners or seizure meds-the FDA looks at real-world data, patient outcomes, and even post-market reports.
It’s not easy. Generic companies spend millions on these tests. The FDA reviews every study. And if something doesn’t add up, the code gets pulled. In 2019, the FDA removed TE ratings from several generic budesonide inhalers after reports showed inconsistent dosing-even though they passed lab tests. That’s how seriously they take this.
Why TE Codes Matter for Your Health and Wallet
Brand-name drugs can cost hundreds or even thousands of dollars a month. Generics? Often under $10. TE codes make that possible. In 2022, generic drugs saved the U.S. healthcare system over $2.2 trillion since 1995, according to the FDA. That’s not a guess-it’s tracked by every prescription filled.
And it works. About 90% of all prescriptions in the U.S. are for generics. Pharmacists substitute them automatically, unless your doctor says "dispense as written." That’s because every state law allows it-thanks to TE codes. Without this system, pharmacists would have to call your doctor every time, slowing things down and raising costs.
Take atorvastatin, the generic for Lipitor. Studies published in JAMA Internal Medicine in 2021 showed no difference in lowering bad cholesterol between brand and multiple TE-rated generics. Patients didn’t feel different. Their labs didn’t change. But their bills did-dropping by 85%.
When TE Codes Don’t Tell the Whole Story
TE codes are powerful, but they’re not perfect. They don’t cover every drug. Single-source generics-those with no brand-name version-are not rated. And some drugs are just harder to copy.
Narrow therapeutic index (NTI) drugs are the biggest concern. These are medicines where a tiny change in dose can cause serious side effects or make the drug stop working. Warfarin (a blood thinner), levothyroxine (for thyroid), and some seizure medications fall into this category. Even if two generics have the same "A" rating, some patients report feeling different when switching between them. A 2022 study found 12.7% of patients noticed changes after switching-even though lab results showed no difference.
Why? Maybe it’s the fillers, the coating, or how fast the pill dissolves. TE codes don’t measure those subtle differences in real life. That’s why many doctors still write "dispense as written" for NTI drugs. It’s not because generics are unsafe-it’s because individual bodies react differently, and the code system can’t account for that.
Complex products like inhalers, patches, and injectables also pose challenges. A generic inhaler might deliver the same amount of drug, but if the spray pattern or particle size is off, it won’t reach the lungs the same way. That’s why the FDA is working on new TE code extensions for biosimilars and complex generics, with updates expected by 2024.
How Pharmacists Use TE Codes Every Day
When a prescription comes in, the pharmacist checks the drug name and strength. If it’s a generic, they look up its TE code in the Orange Book-usually through their pharmacy software, which pulls data directly from the FDA. If the code is "A," they can swap it. If it’s "B," they can’t, and they must call the prescriber.
Most pharmacists say TE codes make their job easier. A 2022 survey by the National Community Pharmacists Association found 91% of pharmacists trust TE ratings. One pharmacist on Reddit said the "AA" code for levothyroxine eliminated insurance disputes-because the code proves the generic is interchangeable.
It’s fast too. Verifying a TE code adds less than 30 seconds to filling a prescription, according to the Pharmacy Technician Certification Board. And pharmacy students learn it in school-98% passed TE code questions on their licensing exam in 2022.

What Patients Should Know
If you’re on a generic drug and feel fine, keep taking it. Don’t assume switching brands means something’s wrong. But if you’ve noticed changes-like new side effects, feeling off, or your condition seeming worse after a switch-talk to your doctor or pharmacist. It might not be the drug. But it’s worth checking.
Don’t panic if your generic looks different. Pills change color, shape, or size all the time. That’s normal. What matters is the TE code. Ask your pharmacist: "Is this generic rated "A"?" They’ll show you.
And if your doctor says "dispense as written," it’s not because they don’t trust generics. It’s because they know your body responds best to one version. That’s personal medicine-and TE codes don’t override that.
The Future of TE Codes
The system isn’t static. The FDA is expanding it. By 2027, they plan to include more complex drugs, use real-world patient data, and create new codes for biosimilars (the next generation of biologic generics). They’re also working on better ways to flag drugs where small differences matter.
Meanwhile, the numbers keep growing. In 2022, generics made up 90.1% of all prescriptions. By 2027, that’s expected to hit 93.4%. And with healthcare costs still rising, TE codes will keep playing a critical role in keeping medicines affordable.
They’re not magic. But they’re reliable. And for most people, most of the time, they work exactly as intended: safe, effective, and cheap.
What does an "A" code mean on a generic drug?
An "A" code means the FDA has determined the generic drug is therapeutically equivalent to the brand-name version. It has the same active ingredient, dosage, strength, route of administration, and bioequivalence-meaning it works the same way in your body. Pharmacists can legally substitute it without a doctor’s approval.
Can I ask my pharmacist to give me the brand-name drug instead of the generic?
Yes. Even if a generic has an "A" rating, you can request the brand-name version. Your pharmacist can fill it, but your insurance may charge you more-or not cover it at all. Some doctors also write "dispense as written" on prescriptions to prevent substitution, especially for drugs like warfarin or levothyroxine.
Are all generic drugs rated with TE codes?
No. Only multi-source drugs-those with at least one brand-name version and one or more generics-are evaluated for TE codes. Single-source generics (with no brand equivalent) don’t get a code. Also, complex products like inhalers, patches, and some injectables may not receive a code if bioequivalence can’t be proven with current methods.
Why do some patients feel different after switching generics?
Even with the same TE code, small differences in inactive ingredients, pill coating, or dissolution rate can affect how a drug is absorbed in some people. This is most common with narrow therapeutic index drugs like warfarin or levothyroxine. While clinical studies show no average difference, individual patients may notice changes in side effects or effectiveness. If this happens, talk to your doctor-staying on the same generic version may be best for you.
Where can I check a drug’s TE code?
The official source is the FDA’s Orange Book, available online at fda.gov/orangebook. Most pharmacy systems automatically display TE codes when filling prescriptions. You can also ask your pharmacist to show you the code for your medication. Apps from the American Pharmacists Association also provide quick access to TE ratings.
What to Do Next
If you’re on a generic medication and have no issues, keep taking it. The system works. If you’ve switched generics and noticed a change-like new side effects, feeling more tired, or your condition worsening-don’t ignore it. Write down what changed, when, and how. Bring it to your doctor or pharmacist. They can check the TE code, see if you’ve switched manufacturers, and decide if staying on one version is better for you.
And if you’re ever unsure whether your drug is rated for substitution, ask. It’s your right to know. TE codes exist to protect you-not to push cheaper drugs on you. When used right, they’re one of the most successful public health tools in modern medicine.










Stacy Foster December 11, 2025
The FDA is totally in bed with Big Pharma-TE codes? Just a scam to push generics so they can charge more for the brand names later. I’ve seen people go into seizures after switching generics. They don’t test real-world outcomes. They test lab rats in a jar. You think they care if your kidney fails? Nah. They just want your insurance to pay less. Wake up.
sandeep sanigarapu December 12, 2025
TE codes are essential for affordable medicine. The system is transparent, science-based, and saves lives daily. In India, we rely on such standards to access quality generics. Trust the process.
Nathan Fatal December 12, 2025
What’s fascinating is how TE codes represent a rare moment where regulatory rigor and market efficiency align perfectly. The FDA didn’t just create a label-they built a trust architecture. Every "A" rating is a promise backed by bioequivalence studies, manufacturing audits, and post-market surveillance. It’s not perfect, but it’s the most rational compromise between access and safety we’ve ever had in pharmacology.
Rob Purvis December 13, 2025
Wait-so if a generic has an "A" rating, that means it’s bioequivalent? But then why do some people say they feel different? Is it placebo? Or is it the excipients? And what about the coating? And the dissolution rate? And the tablet hardness? And the manufacturing batch variance? And the storage conditions? And the patient’s gut microbiome? And the time of day? And the food intake? And the liver enzymes? And the genetic polymorphisms? And the concurrent medications? And the hydration level? And the…
Audrey Crothers December 14, 2025
OMG I switched from one generic to another for my thyroid med last month and I felt like a zombie for two weeks 😭 I thought I was dying!! Then I called my pharmacist and she showed me the TE code-turns out they switched from "AA" to "AB"-and AB isn’t even supposed to be interchangeable!! I demanded my old one back and now I’m fine. TE codes save lives, but only if you know how to read them!! 💪
Reshma Sinha December 15, 2025
TE codes are the backbone of pharmacoeconomic efficiency in emerging markets. The harmonization of bioequivalence parameters with WHO guidelines enables scalable access. Without this framework, formulary decisions would be chaotic.
Lawrence Armstrong December 15, 2025
My dad’s on warfarin. He switched generics once. Didn’t feel different. Labs were fine. But he still takes the same brand. Just in case. 🤷♂️
Donna Anderson December 16, 2025
i had no idea te codes were a thing until my pharmacist told me to ask for the code next time i got a rx. now i always check. no more surprises. also i like that my pills change color lol
Levi Cooper December 17, 2025
Why are we letting foreign manufacturers make our life-saving drugs? TE codes sound great, but half these generics come from China and India where quality control is a joke. We’re trusting our health to factories with no oversight. This isn’t freedom-it’s national security failure.
Adam Everitt December 17, 2025
TE codes are a marvel really, if you think about it-like a barcode for biological trust. But the system’s built on averages, and humans aren’t averages. I’ve seen people react to a different dye in a pill. The code says "A," but the body says "no."
Ashley Skipp December 18, 2025
People complain about generics but they don’t even know what TE codes are. If you don’t like it don’t take them. Simple.
Robert Webb December 20, 2025
I’ve been a pharmacist for 22 years, and I’ve seen TE codes evolve from paper binders to real-time API integrations in our dispensing software. What’s often missed is how this system empowers patients. When someone asks, "Why does this pill look different?"-we can show them the Orange Book entry, explain the equivalence, and reassure them. It’s not just about cost-it’s about transparency. And yes, we do get questions about NTI drugs all the time. That’s why we document every switch, track patient feedback, and never assume. The TE code is a starting point, not the end of the conversation.
nikki yamashita December 21, 2025
Love that generics are cheap and work! 💖 Keep it up!
wendy b December 21, 2025
Actually, the FDA’s TE system is woefully outdated-designed for simple small molecules, not complex biologics or nanoscale formulations. It’s a 1984 framework clinging to 2024 realities. The "A" rating is a relic. We need precision medicine metrics, not population-based bioequivalence thresholds. The system is fundamentally flawed.