When you hear the word DEXA scan, you might think of a complicated medical test reserved for older people with broken bones. But it’s much more than that. For many, it’s the quiet moment that changes everything - the difference between ignoring a silent problem and catching it before it turns into a fracture.
Every year, over 15 million DEXA scans are done in the U.S. alone. Most are for women over 65, but men over 70, people on long-term steroids, or those who’ve had a minor fracture after age 50 are also candidates. The test is quick, painless, and uses less radiation than a cross-country flight. Yet, confusion around the results is common. What does a T-score of -2.1 really mean? Is osteopenia just a warning, or is it already a disease? And why does your doctor care about your height loss or your mom’s hip fracture history?
What a DEXA Scan Actually Measures
A DEXA scan doesn’t just measure how dense your bones are - it measures how much mineral is packed into a specific area of bone, usually the lower spine and hip. The machine sends two very low-dose X-ray beams through your body. One is absorbed by soft tissue, the other by bone. The difference tells the computer exactly how much bone mineral you have per square centimeter - that’s your bone mineral density, or BMD.
It’s not a CT scan. It doesn’t show you 3D images of your bones. It gives you a flat, 2D picture, but one that’s been proven over decades to predict fracture risk better than any other tool. That’s why it’s the gold standard. Other methods, like ultrasound of the heel or peripheral DEXA machines that scan your wrist, are cheaper and more portable. But they don’t measure the spine or hip - the two places where fractures cause the most harm. If you’re being screened for osteoporosis, you need a central DEXA scan.
The radiation? Less than what you get from natural background sources in two days. You could eat a banana or take a flight and get more. There’s no need to fear it. But you should care about the results.
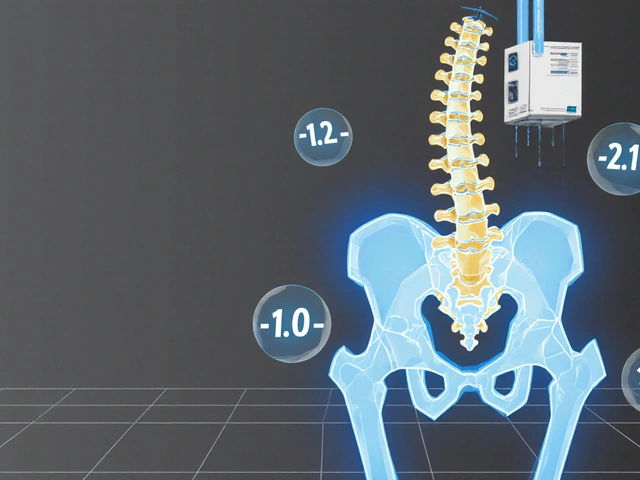
Understanding T-scores and Z-scores
The numbers on your DEXA report aren’t just random digits. They’re standardized comparisons. The most important number is your T-score.
A T-score compares your bone density to the average peak bone density of a healthy 30-year-old adult of your same sex and race. Think of it like this: if your T-score is 0, your bones are as strong as the average 30-year-old’s. If it’s -1.0, you’re 1 standard deviation below that peak. If it’s -2.5, you’re 2.5 standard deviations below.
Here’s what those numbers mean in real terms:
- T-score of -1.0 or higher: Normal bone density. Your bones are in good shape.
- T-score between -1.0 and -2.5: Osteopenia. This isn’t osteoporosis, but it’s a red flag. Your bones are weaker than they should be for your age.
- T-score of -2.5 or lower: Osteoporosis. Your bones are fragile enough that even a minor fall or cough could cause a fracture.
Then there’s the Z-score. This compares your bone density to people your own age, sex, and ethnicity. A Z-score below -2.0 in someone under 50 is unusual. It might mean something else is going on - like a hormone problem, celiac disease, or long-term steroid use. It doesn’t diagnose osteoporosis, but it can point to a hidden cause.
Many people panic when they see “osteopenia.” But it’s not a death sentence. It’s a signal. Something’s off, and you have time to fix it.
Fracture Risk Isn’t Just About Bone Density
Here’s the thing most doctors don’t say out loud: a T-score alone doesn’t tell you if you’ll break a bone. Two people can both have a T-score of -2.3. One falls and breaks a hip. The other never falls at all.
That’s where FRAX comes in. It’s not a machine. It’s a free online calculator developed by the World Health Organization. You plug in your age, sex, weight, height, whether you smoke, if you’ve had a prior fracture, if your mom broke a hip, if you take steroids, if you drink alcohol daily - and it spits out your 10-year risk of a major osteoporotic fracture (hip, spine, forearm, shoulder).
Studies show FRAX improves fracture prediction by 15% to 22% when used with a DEXA scan. A woman with a T-score of -2.1 might have a 10% risk of fracture. But if she’s 75, smokes, drinks two glasses of wine every night, and had a wrist fracture five years ago? Her risk jumps to 28%. That changes everything.
Doctors who only look at the T-score are missing half the picture. The best care combines the scan with your life story.
Who Needs a DEXA Scan?
Not everyone needs one. But if any of these apply to you, you should ask your doctor:
- You’re a woman 65 or older
- You’re a man 70 or older
- You’ve broken a bone after age 50 from a minor fall
- You’re on long-term steroid medication (like prednisone for more than 3 months)
- You have a medical condition linked to bone loss - rheumatoid arthritis, hyperthyroidism, celiac disease, or chronic kidney disease
- You’ve lost more than 1.5 inches in height
- Your mom or dad broke a hip
- You smoke or drink alcohol daily
- You’re underweight (BMI under 19)
Medicare covers a DEXA scan every two years for women 65+ and men 70+ who meet these criteria. Most private insurers follow the same rules. But if you’re under 65 and have risk factors, you may still qualify. Don’t assume you’re too young - bone loss doesn’t care about your age, only your biology.
What the Scan Won’t Tell You
DEXA has limits. It can’t see the inside structure of your bone. Two people with the same T-score can have very different bone quality. One has thick, strong trabeculae (the internal meshwork). The other has thin, broken ones. DEXA can’t tell the difference.
That’s why some clinics now add something called Trabecular Bone Score (TBS). It’s not a separate test. It’s software that analyzes the texture of your spine image during the DEXA scan. A lower TBS means your bone’s internal structure is crumbling - even if the density looks okay. Studies show TBS improves fracture prediction by up to 18%.
Another blind spot? Metal implants. If you’ve had a hip replacement, spinal fusion, or even a large dental filling, the scan can give false readings. Your technician needs to know about these before the test. They’ll adjust the scan or pick a different site.
And then there’s the issue of body size. Very thin people may get falsely low T-scores. Very muscular or overweight people may get falsely high ones. That’s why weight and height matter - they’re part of the FRAX calculation for a reason.
What Happens After the Scan?
If your T-score is normal? Great. Keep doing what you’re doing. Eat enough protein and calcium. Get outside for sunlight. Do strength training twice a week. Avoid smoking and too much alcohol.
If you have osteopenia? This is your wake-up call. You don’t need drugs right away. But you do need action:
- Get 1,200 mg of calcium daily from food or supplements
- Take 800-1,000 IU of vitamin D every day
- Do weight-bearing exercise - walking, dancing, stair climbing, lifting weights
- Quit smoking if you smoke
- Limit alcohol to one drink a day or less
Recheck your DEXA in 1-2 years. If your T-score drops, or your FRAX risk climbs above 20%, your doctor may recommend medication - like bisphosphonates or denosumab. These drugs cut fracture risk by 40-70% in people with osteoporosis.
If you have osteoporosis? Medication is usually recommended. But even then, lifestyle changes are the foundation. No drug works if you’re not moving, not eating, or still smoking.
Real Stories, Real Results
One woman, 68, came in because her hip hurt after a small stumble. Her DEXA showed a T-score of -2.7. She had no symptoms before that. No pain. No history of fractures. But her spine showed signs of a previous, silent compression fracture. She started treatment. A year later, she walked 10,000 steps a day. No new fractures. No pain.
Another man, 72, had a T-score of -2.1. He thought he was fine. But his FRAX score was 24% - higher than his risk of having a heart attack. He started exercise, vitamin D, and a low-dose medication. Two years later, his T-score improved to -1.9. His FRAX dropped to 16%. He’s still hiking.
Osteoporosis doesn’t scream. It whispers. A DEXA scan is how you finally hear it.
Common Questions About DEXA Scans
How often should I get a DEXA scan?
If your first scan is normal and you have no risk factors, you may not need another for 10-15 years. If you have osteopenia, get retested every 1-2 years. If you have osteoporosis and are on treatment, repeat the scan every 1-2 years to check if your bone density is improving or stabilizing. Always follow your doctor’s advice - it depends on your individual risk.
Is the radiation from a DEXA scan dangerous?
No. A typical DEXA scan exposes you to 0.001 to 0.03 millisieverts of radiation. That’s less than you get from natural background sources in two days. A chest X-ray is about 0.1 mSv. A cross-country flight is 0.03-0.05 mSv. The benefit of catching bone loss early far outweighs this tiny risk.
Can I get a DEXA scan if I have a hip replacement?
Yes, but the scan won’t be accurate on the side with the implant. Your technician will skip that hip and focus on the other side, or use your spine instead. Always tell the staff about any metal implants, including spinal rods, screws, or even large dental fillings - they can interfere with the reading.
What’s the difference between osteopenia and osteoporosis?
Osteopenia means your bone density is lower than normal but not low enough to be called osteoporosis. It’s a warning sign. Osteoporosis means your bones are significantly weaker and fracture risk is high. Osteopenia doesn’t always lead to osteoporosis - with the right steps, you can stop it from getting worse.
Do I need to prepare for a DEXA scan?
No special prep is needed. But avoid taking calcium supplements or multivitamins with calcium for 24 hours before the scan. Wear loose, comfortable clothing without metal zippers, buttons, or belts. If you’ve had a barium study or CT scan with contrast in the last week, let your doctor know - you may need to reschedule.
Next Steps: What to Do Now
If you’re over 65, or have risk factors, don’t wait for symptoms. Ask your doctor for a DEXA scan. If you’ve had one already and don’t understand your results, bring the report to your next appointment. Write down your T-score and FRAX score. Ask: “What does this mean for my risk of breaking a bone?”
Don’t let confusion stop you. Bone health isn’t about being old. It’s about being informed. The sooner you know your numbers, the more control you have over your future.





Manish Pandya November 26, 2025
Just got my DEXA results back-T-score of -1.8. Was freaking out until I read this. Turns out I’m not doomed, just… mildly disappointed in my skeleton. Time to start lifting weights and stop treating my couch like a second home.
Adesokan Ayodeji November 27, 2025
Man, this is the kind of post that makes me believe in the internet again. Seriously-bone health isn’t just for grandmas. I’m 52, never thought I’d care about T-scores, but after my dad broke his hip last year, I got scanned. Turns out I had osteopenia. Started walking 30 minutes a day, took vitamin D, cut out soda. My last scan? Up to -1.2. It’s not magic, it’s just consistency. You don’t need to be perfect, just persistent. Your future self will thank you.
Benjamin Gundermann November 27, 2025
Look, I get it-bone density is important. But let’s be real, this whole osteoporosis panic is just Big Pharma’s way of selling pills to people who don’t want to admit they’re aging. I’m 67, I’ve never broken a bone, I eat cheese and drink milk, and I still hike. Why are we turning a natural part of aging into a medical emergency? They scan you, scare you, then sell you a $200-a-month drug that gives you jaw rot. I’d rather just live and die on my own terms, thanks.
Karen Ryan November 29, 2025
OMG I JUST GOT MY RESULTS!! 😱 T-score -2.3 😭 I thought I was fine because I’m active… but now I’m crying in the grocery store aisle next to the calcium supplements. Anyone else feel like their bones betrayed them?? 🥺
Terry Bell November 29, 2025
Man, I love how this breaks it down. I’m 61, had a wrist fracture last year after tripping on my own dog. Didn’t think much of it-until my doc said, ‘Hey, that’s not normal for someone your age.’ Got the DEXA, T-score was -2.1, FRAX was 27%. Scared me straight. Now I do squats with water bottles, take D3, and I don’t even drink wine anymore. My dog’s still a menace, but my bones? They’re catching up. You’re not too late. Ever.
Lawrence Zawahri November 30, 2025
They’re lying to you. DEXA scans? Total scam. The government and the radiology industry are pushing this because they want to track your bone density like it’s a surveillance tool. Why do they need your spine data? What are they building? And why is vitamin D so cheap but bisphosphonates cost a fortune? Wake up. The real cause of bone loss? Fluoride in the water. Glyphosate. 5G. They don’t want you to know that. They want you dependent on drugs. I’ve stopped all scans. I eat dirt. I’m stronger than ever.
Rachelle Baxter December 2, 2025
Ugh. I can’t believe people still think osteopenia isn’t a disease. It’s literally the precursor to osteoporosis. If you ignore it, you’re just gambling with your future mobility. And don’t even get me started on those who say ‘I’m fine because I walk.’ Walking doesn’t build bone density. Resistance training does. And if you’re not doing it, you’re just delaying the inevitable. Stop making excuses. Your spine isn’t a suggestion.
Dirk Bradley December 2, 2025
While the article presents a superficially coherent exposition on bone mineral density assessment, one must acknowledge the inherent epistemological limitations of dual-energy X-ray absorptiometry. The reductionist quantification of skeletal integrity via T-scores neglects the complex biomechanical heterogeneity of trabecular architecture. Moreover, the uncritical adoption of FRAX as a predictive instrument reflects a troubling conflation of statistical probability with clinical necessity. One ought to interrogate the institutional incentives underlying the proliferation of these screening protocols-particularly in populations where pharmaceutical intervention is disproportionately promoted over holistic, lifestyle-based remediation.
Emma Hanna December 3, 2025
Wait. Wait. Wait. You’re telling me that if I have a T-score of -1.5, and I’ve never had a fracture, and I’m 58, I’m still at risk? And you’re telling me I need to take calcium supplements? But I’m lactose intolerant! And I hate yogurt! And my doctor said I don’t need it! What if I just… eat more kale? Isn’t that enough? Why does everyone keep pushing pills? I’m not a lab rat!
Mariam Kamish December 4, 2025
So I got my DEXA. T-score: -2.0. FRAX: 21%. I’m supposed to be ‘concerned.’ But honestly? I’ve been doing yoga for 10 years. I don’t smoke. I drink wine. I’m not fat. I don’t feel weak. Why am I being punished for being a normal person who just… lives? This feels like victim-blaming disguised as medicine.