When you’re managing diabetes and start noticing strange new symptoms-like unexplained weight gain, constant fatigue, or mood swings-it’s easy to blame it all on your blood sugar. But what if part of the problem isn’t diabetes at all? What if your thyroid is quietly throwing your whole system off balance?
It’s more common than you think. About 1 in 3 people with diabetes also have a thyroid disorder. And nearly 1 in 7 people with thyroid problems also have diabetes. These aren’t separate issues. They’re linked. The same autoimmune mistakes that attack your pancreas in Type 1 diabetes can also target your thyroid. Even in Type 2 diabetes, thyroid hormones directly influence how your body uses insulin and processes sugar.
Why Your Thyroid Affects Your Blood Sugar
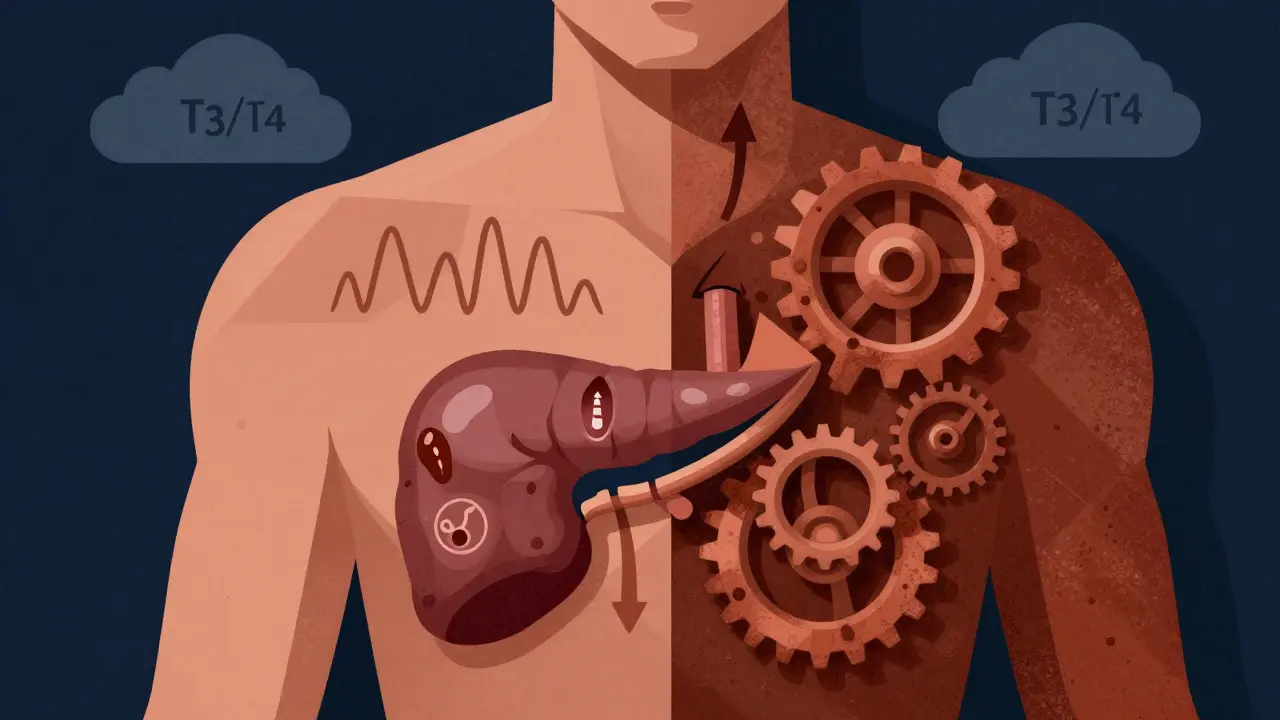
Your thyroid doesn’t just control metabolism-it controls how fast or slow your body turns food into energy. That includes glucose. When your thyroid is underactive (hypothyroidism), your body slows down. Glucose gets cleared from your blood more slowly. Insulin doesn’t work as well. Blood sugar stays high, even if you’re eating right and taking your meds. Studies show hypothyroidism can reduce glucose metabolism by 25-30%, making insulin resistance worse.
On the flip side, an overactive thyroid (hyperthyroidism) speeds everything up. Your liver dumps glucose into your bloodstream faster. Your muscles burn through sugar quicker. Your body clears insulin faster too-up to 25% more. That means if you’re on insulin, your usual dose might suddenly cause low blood sugar. Or worse, you might need 30% more insulin just to keep up.
One patient from Tampa Bay, diagnosed with Type 1 diabetes at 19, saw her insulin needs drop by 30% after being diagnosed with hypothyroidism. She had three dangerous low-blood-sugar episodes in a week before her doctor adjusted her dose. That’s not rare. It’s a red flag.
Symptoms That Look Like Diabetes-But Aren’t
Here’s the tricky part: the symptoms of thyroid disease and diabetes overlap so much, even doctors sometimes miss the connection.
- Weight changes: Unexplained weight gain? Could be hypothyroidism. Rapid weight loss despite eating more? Could be hyperthyroidism. Both happen in 65-70% of people with both conditions.
- Fatigue: Feeling wiped out even after sleeping? 78% of people with both diabetes and thyroid disease report this. It’s not just high blood sugar.
- Hair loss: Thinning hair or patchy eyebrows? Thyroid-related. It’s not just stress or aging.
- Mood swings and depression: Feeling down, anxious, or emotionally numb? Thyroid hormones affect serotonin and dopamine. 55% of patients with both conditions report mood issues.
- Temperature sensitivity: Always cold? Hypothyroidism. Sweating through your clothes in a cool room? Hyperthyroidism. 61% of patients report this.
- Memory problems: Forgetting where you put your keys or why you walked into a room? 45% of patients with both conditions report brain fog.
And here’s the silent danger: hypothyroidism can hide low blood sugar. Normally, when your blood sugar drops, your body releases adrenaline. You feel shaky, sweaty, your heart races. But if your thyroid is underactive, that adrenaline response is blunted. You might pass out before you even feel the warning signs. One study found 41% of diabetic patients with untreated hypothyroidism had unrecognized hypoglycemia.

What Your Doctor Should Be Testing
If you have diabetes, your thyroid isn’t something you check once and forget. It needs regular monitoring.
The American Diabetes Association recommends annual TSH testing for all Type 1 diabetes patients and high-risk Type 2 patients. But that’s the bare minimum. If you’re already showing symptoms, or if your blood sugar is harder to control than it should be, ask for more:
- TSH (Thyroid Stimulating Hormone) - the first line test
- Free T4 and Free T3 - to see actual hormone levels
- Thyroid antibodies (TPOAb and TgAb) - to catch autoimmune thyroid disease early
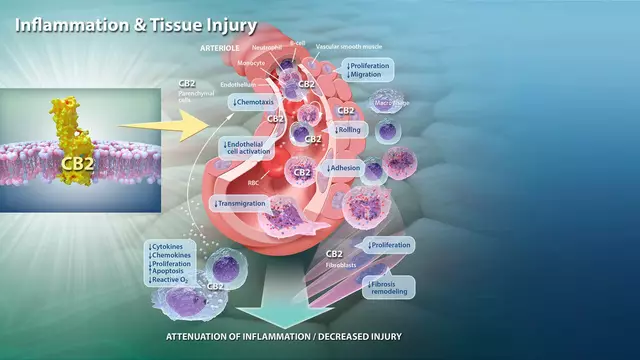
Patients with Type 1 diabetes are 5 to 10 times more likely to develop autoimmune thyroid disease than the general population. That’s not a coincidence. It’s genetics. Your immune system is already on the hunt for insulin-producing cells. It might turn its attention to your thyroid next.
And don’t wait for symptoms. Some people have subclinical hypothyroidism-TSH is slightly high, but T4 is normal. That’s still enough to worsen insulin resistance and raise your risk of diabetic retinopathy by 37%. A 2024 study found these patients had higher rates of eye damage, even if their blood sugar seemed okay.
Medication and Lifestyle Adjustments
Taking levothyroxine for hypothyroidism sounds simple. But if you have diabetic neuropathy, your stomach might move food slowly (gastroparesis). That can cut levothyroxine absorption by 15-20%. You might need to take it on an empty stomach, 30-60 minutes before breakfast, and avoid coffee or calcium supplements for hours after.
And your diabetes meds? They might need tweaking too. If you’re on insulin and your thyroid starts working better, your insulin needs could drop suddenly. That’s not a win-it’s a risk. One patient on Reddit said her endocrinologist didn’t adjust her insulin after her thyroid levels normalized. She ended up in the ER with severe hypoglycemia.
Lifestyle changes help both conditions at once:
- Mediterranean diet: Rich in olive oil, fish, vegetables, nuts, and whole grains. In a 6-month study, this diet lowered HbA1c by 0.8-1.2% and improved TSH levels by 0.5-0.7 mIU/L.
- Regular exercise: Even 30 minutes of walking daily improves insulin sensitivity and thyroid hormone conversion.
- Stress management: Chronic stress raises cortisol, which worsens both insulin resistance and thyroid function.
Continuous glucose monitors (CGMs) are game-changers for people with both conditions. A 2022 JAMA study showed CGM users had 32% fewer low-blood-sugar events and 27% better time-in-range than those using fingersticks. Why? Because you can see patterns-like if your sugar drops after meals or spikes overnight-and link them to thyroid fluctuations.

The Cost of Ignoring the Connection
Ignoring thyroid problems when you have diabetes isn’t just risky-it’s expensive. People with both conditions spend an extra $4,872 per year on healthcare. Why? More hospital visits, more emergency care, more complications like nerve damage, kidney disease, and heart problems.
Thyroid disease also raises LDL cholesterol by 18-22 mg/dL and triglycerides by 25-30 mg/dL. That’s a one-two punch for your heart. Diabetic patients with untreated hypothyroidism are at higher risk for heart attacks and strokes.
And here’s the kicker: 58% of patients with both conditions report at least one medication error because doctors didn’t realize the symptoms were overlapping. 22% needed hospitalization because of it.
What’s Changing in 2025
Doctors are finally catching up. New guidelines from the American Association of Clinical Endocrinologists, set to release in late 2024, will include specific algorithms for managing thyroid dysfunction in Type 1, Type 2, and gestational diabetes. For the first time, there will be clear protocols for when to test, how often to recheck, and how to adjust meds.
Emerging research is even more promising. A 2024 pilot study found that GLP-1 receptor agonists-meds like semaglutide used for diabetes-actually improved thyroid function in 63% of patients with subclinical hypothyroidism. The NIH is now running a 5,000-person study called TRIAD to see if treating thyroid issues early can delay or even prevent diabetes in high-risk people.
Integrated care isn’t the future. It’s the present. If you have diabetes and your symptoms don’t quite add up, ask about your thyroid. Don’t wait for your annual checkup. If your blood sugar is erratic, your energy is gone, or you’re losing hair for no reason, it’s time to test.
Managing both conditions together isn’t harder-it’s smarter. When you treat the thyroid, your diabetes becomes easier to control. Your energy comes back. Your mood improves. Your risk of complications drops. And you stop guessing why you feel so awful.
Can thyroid problems cause high blood sugar?
Yes. Hypothyroidism slows down how your body uses glucose, leading to insulin resistance and higher blood sugar levels. Studies show it can reduce glucose metabolism by 25-30%. Even if you’re eating well and taking your diabetes meds, an underactive thyroid can make your blood sugar harder to control.
Can diabetes cause thyroid problems?
Type 1 diabetes and autoimmune thyroid disease share the same root cause: your immune system attacks your own tissues. If you have Type 1 diabetes, you’re 5-10 times more likely to develop Hashimoto’s or Graves’ disease. Type 2 diabetes can also affect thyroid function by altering how your body converts T4 to T3 and raising TSH levels over time.
Should I get my thyroid checked if I have diabetes?
Yes. The American Diabetes Association recommends annual TSH testing for all Type 1 diabetes patients and high-risk Type 2 patients. If you have symptoms like fatigue, weight changes, or hair loss-even if your blood sugar is stable-ask for a full thyroid panel, including TPO antibodies.
Can levothyroxine affect my blood sugar?
Yes. When you start levothyroxine, your metabolism speeds up. This can increase insulin sensitivity, which may cause your blood sugar to drop. If you’re on insulin or other glucose-lowering meds, your dose may need to be lowered within days of starting thyroid treatment. Always monitor your blood sugar closely during the first few weeks.
Why do I feel worse even though my blood sugar is normal?
You might have an undiagnosed thyroid issue. Symptoms like fatigue, brain fog, hair loss, and cold intolerance aren’t always caused by blood sugar. If your thyroid is underactive, your body isn’t producing enough energy-even if your glucose levels look good on paper. A simple TSH test can reveal the real culprit.




Jocelyn Lachapelle December 15, 2025
I had no idea my fatigue wasn't just from diabetes. Started testing my thyroid after months of feeling like a zombie and turns out my TSH was through the roof. Levothyroxine changed everything. Energy back. Mood stable. No more 3pm crashes.
Just sayin'.
John Samuel December 16, 2025
This is precisely why integrative endocrinology must become the standard of care. The confluence of autoimmune dysregulation in Type 1 diabetes and thyroid pathology is not merely coincidental-it is mechanistically inevitable. One must interrogate the entire hypothalamic-pituitary-thyroid-adrenal axis, not merely isolate glucose metrics. A TSH alone is insufficient; one must evaluate Free T3, Free T4, and thyroid peroxidase antibodies to achieve clinical precision.
Sai Nguyen December 16, 2025
Americans always overcomplicate everything. Just test TSH. Take pill. Stop complaining.
Michelle M December 18, 2025
It’s funny how we treat symptoms like separate enemies when the body’s just trying to tell us something’s out of balance. Thyroid and pancreas aren’t rivals-they’re partners in a system that got loud because we stopped listening. Maybe healing isn’t about more meds, but about remembering we’re one organism, not a checklist of organs.
Cassie Henriques December 20, 2025
Fascinating. The T4-to-T3 conversion impairment in insulin resistance is underappreciated. Peripheral deiodinase activity (DIO2) is downregulated in adipose tissue under chronic hyperglycemic stress, leading to functional hypothyroidism even with normal TSH. That’s why some patients on levothyroxine still feel awful-T4 isn’t the issue, T3 bioavailability is. Consider adding liothyronine in refractory cases.
Jake Sinatra December 20, 2025
I’ve seen this too many times. Patient comes in with erratic glucose, blames insulin, refuses to check thyroid. Then we test-TSH 8.7. Start levothyroxine. Insulin dose drops 40%. No more nocturnal lows. This isn’t alternative medicine. It’s physiology. Why isn’t this routine?
RONALD Randolph December 22, 2025
You people need to stop ignoring the facts! The ADA says TSH annually-so why are you waiting for symptoms?! You’re not 'just tired'-you’re hypothyroid! And if you're on coffee or calcium with your levothyroxine? You're sabotaging yourself! Stop making excuses and test your thyroid! It's not hard!
Benjamin Glover December 23, 2025
How quaint. Another American medical article that mistakes complexity for insight. In the UK, we test TSH at diagnosis and move on. The rest is overdiagnosis dressed as innovation.
Raj Kumar December 23, 2025
Bro i had same issue. Was on 50u insulin daily, felt like death. Got TSH checked, was 6.2. Started levothyroxine 50mcg. After 2 weeks, insulin down to 35u. No more dizzy spells. Also started walking daily. Life changed. Don't ignore it.
Melissa Taylor December 24, 2025
This is the kind of info I wish my doctor had told me two years ago. I thought my hair loss was stress. Turns out it was my thyroid. I feel like a new person now. Thank you for writing this.
John Brown December 24, 2025
I’ve been telling my diabetic friends for years: if your blood sugar’s 'fine' but you still feel awful, get your thyroid checked. It’s not a stretch. It’s basic. And if your doc says 'wait till next year'? Find a new doc. You deserve better.
Christina Bischof December 24, 2025
I didn't realize how much brain fog was from my thyroid. I'd walk into a room and forget why. Now I take my pill on an empty stomach, no coffee for an hour. My focus is back. Just... small things. But they matter.
Mike Nordby December 24, 2025
The 2024 TRIAD study is promising, but we must be cautious. Correlation does not imply causation. While early thyroid intervention may reduce diabetes risk, we lack long-term RCT data. Until then, we should adhere to evidence-based guidelines-not hype-driven protocols.
Lisa Davies December 26, 2025
I started CGM after my thyroid diagnosis and wow-saw my sugar dip 30 mins after eating when my TSH was high. No one told me that. Now I adjust meals around it. Life-changing 💪
Nupur Vimal December 27, 2025
Everyone thinks thyroid is just about TSH but you need to know your antibodies too. If you have type 1, you’re already autoimmune. You think your body won’t attack your thyroid next? Wake up. This isn’t optional. It’s survival.