Renal Dosing Calculator for Elderly Patients
Calculate Adjusted Doses
When you’re over 65 and your kidneys aren’t working like they used to, even a normal dose of a common medication can become dangerous. It’s not about taking too much-it’s about your body not being able to clear it the way it once did. About 38% of adults over 65 have chronic kidney disease, and for many, that means their meds need to change. A simple pill for blood pressure, gout, or diabetes can build up in the system and cause falls, confusion, or even hospitalization. The fix isn’t always obvious, and too often, it’s ignored.
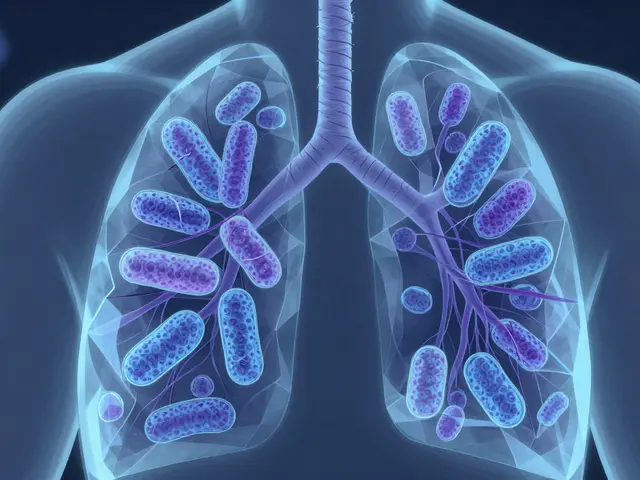
Why Kidneys Matter More as You Age
Your kidneys filter waste, balance fluids, and help control blood pressure. As you get older, kidney function naturally slows. That’s normal. But when the glomerular filtration rate (GFR) drops below 60 mL/min/1.73 m², it’s no longer just aging-it’s renal impairment. At this point, drugs that your kidneys usually clear start sticking around. For some medications, that means levels in your blood can be 50% to 100% higher than intended. That’s not a small change. That’s the difference between a safe dose and a toxic one.Think of it like a clogged drain. If water flows in at the same rate but can’t drain out, the tub overflows. That’s what happens with medications. Even if you take the same pill you’ve taken for years, your body can’t keep up. The result? Side effects that look like dementia, weakness, or heart rhythm problems-when they’re really just drug toxicity.
How Doctors Measure Kidney Function
You can’t guess kidney function by how you feel. You need numbers. The two most common ways to estimate it are the Cockcroft-Gault equation and the MDRD equation. Both use your age, weight, sex, and blood creatinine level. But they don’t give the same answer.The Cockcroft-Gault equation, created in 1976, is still widely used because it’s more conservative. It tends to estimate kidney function lower than it actually is in older adults-by about 15-20%. That sounds bad, but in this case, being overly cautious saves lives. If your creatinine is 1.2 mg/dL, age 78, and you weigh 65 kg, Cockcroft-Gault might give you a CrCl of 42 mL/min. MDRD might say 51. Which one do you trust? For elderly patients, guidelines say go with the lower number. It’s safer.
There’s a newer option: cystatin C. It’s a blood marker that’s less affected by muscle mass, which declines with age. If your creatinine looks normal but you’re frail or thin, cystatin C gives a clearer picture. It’s not available everywhere yet, but it’s becoming the gold standard for older adults.
Medications That Need Special Care
Not all drugs are equal. Some are cleared mostly by the kidneys. Others are broken down by the liver. But even liver-metabolized drugs can have active parts that your kidneys clear. That’s where things get tricky.Here are the big ones that demand attention:
- Metformin: Used for diabetes, it’s generally safe-but only if your kidneys are working. If your CrCl is below 30 mL/min, you shouldn’t take it. Even between 30-45 mL/min, use with extreme caution. Some U.S. doctors still use outdated creatinine cutoffs (1.5 mg/dL for men), but current guidelines focus on GFR, not creatinine alone.
- Gabapentin: Often prescribed for nerve pain or seizures. It’s almost entirely cleared by the kidneys. A standard dose of 300 mg three times a day can become toxic in someone with CrCl under 50 mL/min. The fix? Cut the dose in half or stretch out the timing. Many patients end up confused or dizzy because their dose was never adjusted.
- Allopurinol: For gout. The usual dose is 100 mg daily. But if your GFR is below 10 mL/min, you need to start with 100 mg every other day. Too much can cause a rare but deadly skin reaction.
- Digoxin: Used for heart rhythm. The therapeutic range is narrow: 0.8-2.0 ng/mL. Too low, and it doesn’t help. Too high, and it can stop your heart. Levels should be checked 15-20 days after starting or changing dose in elderly patients with kidney issues-not 5 days like in younger people.
- Lithium: For bipolar disorder. It’s a classic example of a drug with a tiny safety window. Levels above 1.2 mmol/L can be toxic. In elderly patients, even small drops in kidney function can push levels into danger. Regular blood tests aren’t optional-they’re life-saving.
- Antibiotics like cefepime and cefdinir: Cefepime is usually given every 6 hours. But if your CrCl is under 30 mL/min, you need it every 12 hours. Below 10 mL/min? Every 24 hours. Cefdinir drops from twice daily to once daily. Miss this, and you risk seizures or kidney damage.

The 50% Rule-And Why It Fails
Many clinicians use a simple trick: if a drug is more than 50% cleared by the kidneys, cut the dose by half when CrCl drops below 50 mL/min. It’s easy. It’s fast. And it’s often wrong.Drugs like vancomycin don’t follow linear rules. Their clearance changes unpredictably in kidney disease. A 50% reduction might leave you underdosed, risking infection. Or it might still be too much, leading to hearing loss or kidney damage. Gabapentin and rivaroxaban also don’t play nice with oversimplified rules. That’s why blanket approaches fail in 22% of high-risk cases.
The better method? Know your drug. Look up its specific dosing guidelines. Don’t rely on memory. Use a trusted reference-like the University of Nebraska Medical Center’s antimicrobial dosing guide or the Royal Australian College of General Practitioners’ AFP journal. These aren’t just suggestions. They’re based on real patient outcomes.
What Works in Real Life
Knowing what to do is one thing. Doing it consistently is another. A 2015 study found that only 43.7% of doctors regularly adjusted doses for elderly patients with kidney impairment. The biggest mistakes? Gabapentin, rivaroxaban, and allopurinol. These are common prescriptions. And they’re dangerous when mismanaged.Some places are fixing this. At the University of Nebraska Medical Center, they added alerts to their electronic health record system. When a doctor orders cefepime for a patient with CrCl under 30, the system pops up: “Dose adjustment required. Consider 1g IV q12h.” Within a year, inappropriate dosing dropped by 37.2%.
Even better? Pharmacists. At Mayo Clinic, when clinical pharmacists took over dosing for patients over 65 with kidney issues, adverse drug events dropped by 58%. Pharmacists don’t just check doses-they catch drug interactions, question outdated prescriptions, and talk to patients about side effects. They’re the missing link.
Tools to Help You Get It Right
You don’t need to memorize every dosing rule. Tools exist to do the math for you.- Epocrates Renal Dosing: A mobile app used by over 1.2 million clinicians. Type in the drug and the patient’s CrCl, and it gives you the adjusted dose. It’s free, quick, and updated regularly.
- Electronic Health Record (EHR) Calculators: Many systems now auto-calculate CrCl when a creatinine result comes in. Some even suggest dose changes. But not all do it well. Make sure your system uses Cockcroft-Gault, not just MDRD, for elderly patients.
- DoseOptima: The first AI-powered renal dosing platform approved by the FDA in 2023. It pulls data from your EHR, calculates GFR using cystatin C if available, and recommends exact doses for over 150 medications. In a trial of 15,000 patients, it was 92.4% accurate.
These aren’t luxury tools. They’re safety nets. If your doctor doesn’t use them, ask why.

What’s Changing in 2026
Guidelines are catching up. The Kidney Disease: Improving Global Outcomes (KDIGO) group is releasing an updated drug dosing report in late 2023, and it’s already influencing practice. Cystatin C is now recommended as the first-line test for elderly patients, not creatinine alone. The American Society of Health-System Pharmacists is finalizing a national standard for renal dosing across 150 high-risk drugs. And the FDA now requires all new medications targeting people over 65 to include clear renal dosing instructions on the label.Medicare and Medicaid are also stepping in. Hospitals that have too many drug-related falls or poisonings lose up to 1% of their Medicare payments. That’s real money. So institutions are finally investing in better systems.
But the biggest gap? Long-term care facilities. Only 28% of nursing homes have formal renal dosing protocols. That’s where many elderly patients live-and where mistakes are most common.
What You Can Do
If you or someone you care for is over 65 and takes multiple medications:- Ask for a kidney function test. Request the Cockcroft-Gault calculation, not just creatinine.
- Get a full medication review. Bring all your pills-prescription, over-the-counter, supplements-to your doctor or pharmacist.
- Ask: “Is this dose right for my kidneys?” Don’t be shy. This isn’t a dumb question. It’s the most important one.
- Watch for side effects: confusion, dizziness, nausea, muscle weakness, irregular heartbeat. These aren’t just signs of aging. They could be drug toxicity.
- Use a pill organizer with clear labels. If you’re taking a drug like gabapentin or allopurinol, make sure you’re not taking it twice a day when you should be taking it every other day.
Medication safety in older adults isn’t about doing more. It’s about doing less-wisely. Sometimes, the best treatment is stopping something that’s no longer safe.
How do I know if my kidney function is low?
Your doctor can estimate your kidney function using a blood test for creatinine and your age, weight, and sex. The result is called your estimated GFR or CrCl. If your GFR is below 60 mL/min/1.73 m² for three months or more, you have chronic kidney disease. For older adults, even a GFR of 45-59 can mean your medications need adjustment. Ask for the Cockcroft-Gault calculation-it’s more accurate for seniors.
Can I still take metformin if I have kidney problems?
It depends. If your CrCl is below 30 mL/min, you should not take metformin. Between 30-45 mL/min, you can take it but only with close monitoring and a reduced dose. Many doctors still use outdated creatinine cutoffs, but current guidelines say GFR is what matters. Never stop metformin on your own-talk to your doctor about alternatives like glipizide or insulin if needed.
Why is gabapentin dangerous for elderly patients with kidney issues?
Gabapentin is removed almost entirely by the kidneys. In someone with poor kidney function, it builds up and causes dizziness, confusion, falls, and even breathing problems. A standard dose of 300 mg three times a day can become toxic. The fix is simple: reduce the dose or space out the timing. For CrCl under 50 mL/min, cut the dose in half or take it once daily. Many elderly patients are still on full doses because no one checked their kidney function.
What’s the safest pain reliever for someone with kidney problems?
Avoid NSAIDs like ibuprofen or naproxen-they can worsen kidney function. Acetaminophen (Tylenol) is usually the safest choice for short-term pain, as long as you don’t exceed 3,000 mg per day. For chronic pain, non-drug options like physical therapy or heat therapy are better. Always check with your doctor before taking any pain reliever, even over-the-counter ones.
Should I get my lithium levels checked more often if I’m older?
Yes. Lithium has a very narrow safety range. Even small changes in kidney function can cause levels to rise dangerously. In elderly patients, check levels 15-20 days after starting or changing the dose, and then every 3-6 months. If you’re dehydrated, sick, or start a new medication, get tested sooner. Lithium toxicity can cause tremors, confusion, seizures, or coma-none of which are normal aging.
Can I use over-the-counter kidney function tests?
No. Home urine strips or digital kits can’t measure GFR or CrCl accurately. They might detect protein or blood in the urine, but they can’t tell you how well your kidneys are filtering drugs. Only a blood test with a proper calculation by your doctor gives you reliable numbers. Don’t rely on apps or home tests for medication safety.
What if my doctor won’t adjust my meds?
Ask for a referral to a pharmacist who specializes in geriatrics or medication therapy management. Many clinics have these services, especially in hospitals or Medicare Advantage plans. Pharmacists can review your entire list of medications and recommend changes your doctor can approve. You have the right to a second opinion-your safety matters more than convenience.
Next Steps: Protect Yourself
The system isn’t perfect. But you don’t have to wait for it to fix itself. Take charge. Get your kidney numbers. Review your meds. Ask questions. Keep a list of everything you take-including vitamins and supplements-and bring it to every appointment. If you’re on any of the high-risk drugs we mentioned, don’t assume your dose is safe just because it’s the same as last year.Medication toxicity in older adults isn’t inevitable. It’s preventable. And it starts with one question: “Is this dose right for my kidneys?”





ellen adamina January 16, 2026
This hit home. My mom was on gabapentin for years and no one ever checked her kidney function. She started falling constantly - we thought it was just old age. Turned out her dose was triple what it should’ve been. Took three doctors and a pharmacist to catch it.
Now she’s on half the dose and barely needs a cane. Just ask. Always ask.
Mike Berrange January 17, 2026
Let’s be real - this is just another way for Big Pharma to sell more tests and apps. The real problem? Doctors don’t care. They’re paid by volume, not outcomes. And now they’re pushing this cystatin C nonsense because it’s more expensive. Same drugs. Same side effects. Just more billing codes.
Jami Reynolds January 19, 2026
It’s not just about dosing. The entire medical infrastructure is designed to ignore elderly patients. The FDA doesn’t require adequate geriatric trials. Insurance denies coverage for pharmacist consultations. EHR systems use outdated formulas. This isn’t negligence - it’s systemic devaluation of older lives.
And now they want us to trust AI platforms like DoseOptima? Who coded those algorithms? Who owns the data? This isn’t innovation - it’s surveillance with a stethoscope.
Crystel Ann January 20, 2026
I love how you laid this out. So clear. So necessary. My dad’s on lithium and we’ve been checking his levels every 3 months since last year - his neurologist actually thanked us for being proactive. It’s scary how many people just keep taking the same pills forever without a second thought.
Thank you for writing this. It’s the kind of post that saves lives.
Nat Young January 21, 2026
38% of older adults have CKD? That’s a made-up number. The CDC says it’s 14%. You’re conflating eGFR decline with disease. Also, Cockcroft-Gault overestimates risk? No - it’s the only formula that doesn’t assume elderly people are magically healthy. MDRD is for young athletes, not 80-year-olds with sarcopenia.
And DoseOptima? AI that’s 92% accurate? That means 1 in 13 doses is wrong. That’s not a safety net - it’s a roulette wheel with a stethoscope.
Niki Van den Bossche January 22, 2026
Oh, the tragic ballet of pharmacological oblivion - the body, a temple of diminishing returns, slowly dissolving under the weight of industrial medicine’s indifferent algorithms. We’ve turned human frailty into a spreadsheet, and now we sell algorithms to fix the very systems that created the problem.
Is it not poetic that we use the language of cold calculus to manage the warmth of our dying? Cystatin C whispers the truth: we are not machines. We are ghosts in the machine, and the machine forgets us first.
Iona Jane January 24, 2026
They’re lying about the 1% Medicare penalty. It’s a myth. I work in hospital admin - no one’s losing money over this. It’s all smoke and mirrors to push more EHR upgrades. And those pharmacist-led interventions? They’re just replacing doctors because insurance won’t pay for MD time anymore. This isn’t patient care - it’s cost-shifting dressed up as progress.
Jaspreet Kaur Chana January 25, 2026
Bro, I’m from India and we don’t even have access to half this stuff. My uncle in Delhi is on metformin and his doctor just says ‘take one tablet’ - no GFR test, no nothing. We don’t have Epocrates or cystatin C. We have WhatsApp groups with retired nurses and Google Translate.
But you know what? We still ask questions. We still bring all the bottles. We still say ‘Is this safe?’ - because no one else will.
Don’t let the fancy tools make you feel like you need them. You just need to care. And that’s free.
Haley Graves January 27, 2026
THIS. Right here. This is the exact conversation we need to be having. I’m a nurse and I see this every shift. A 78-year-old on 300mg gabapentin three times a day - because ‘it’s what she’s always taken.’
Don’t wait for the system to fix itself. Print this out. Bring it to your doctor. Ask for the Cockcroft-Gault. Say ‘I’m not asking - I’m demanding.’ You deserve to live without being poisoned by your own meds.
Diane Hendriks January 28, 2026
Why are we letting foreign guidelines dictate American medicine? KDIGO? That’s a UN-backed group with no accountability. And now we’re supposed to trust AI from Silicon Valley to dose our grandparents? This isn’t science - it’s cultural surrender. We used to trust our doctors. Now we trust apps written by 22-year-olds who don’t know what a kidney does.
Sohan Jindal January 28, 2026
My dad died from a bad dose. They gave him cefepime like he was 40. He had a seizure in the ER. They said ‘it was just a stroke.’ It wasn’t. It was the antibiotic. No one checked his CrCl. He was 79. They didn’t care. Now I don’t trust any doctor. Not one.