Imagine breaking out in tiny, itchy bumps within minutes of starting a workout, walking to the bus, or even eating a spicy meal. For people with cholinergic urticaria, this isn’t rare-it’s daily. This condition, often called heat hives, isn’t caused by an allergy to heat itself, but by your body’s overreaction to a rise in core temperature. It’s not just an annoyance. For many, it’s a hidden barrier to normal life-canceling workouts, avoiding social events, or even skipping meals because of fear of the next flare-up.
What Exactly Is Cholinergic Urticaria?
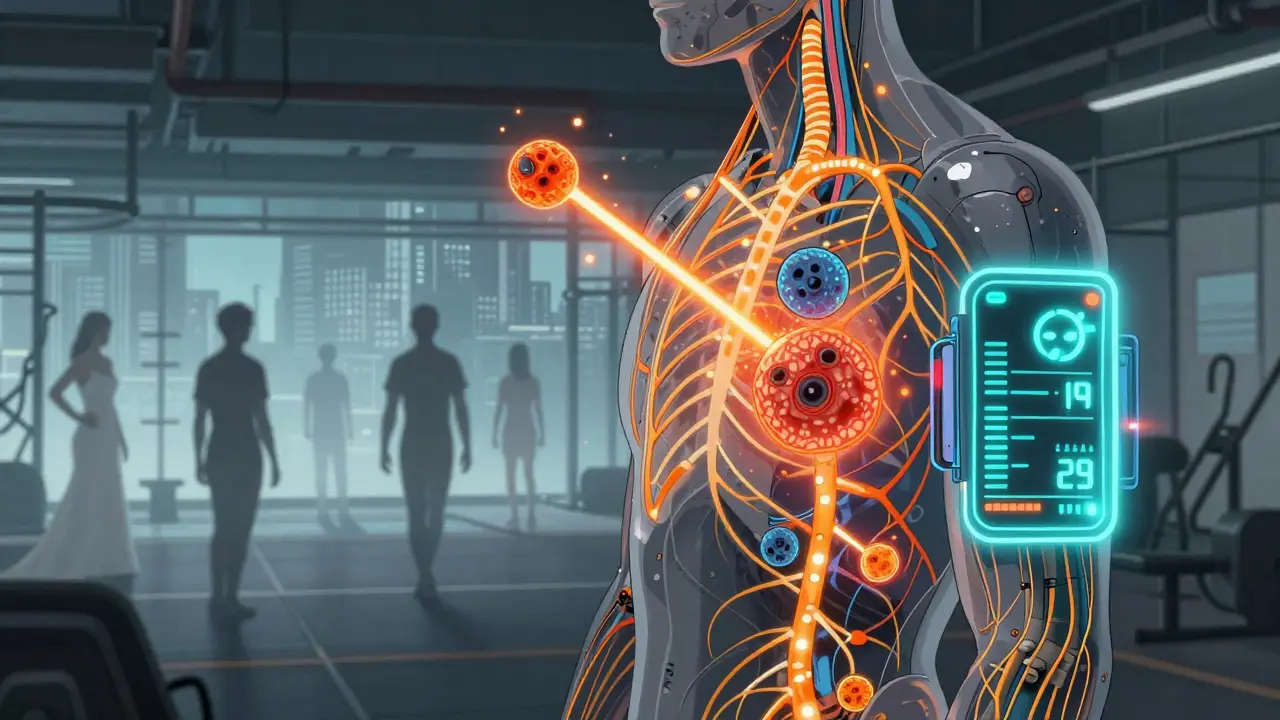
Cholinergic urticaria (CU) is a type of physical urticaria triggered by an increase in body temperature. It’s not an allergic reaction to something you touch or eat. Instead, it’s your nervous system and immune system miscommunicating. When you sweat-whether from exercise, hot weather, stress, or even a hot shower-nerve fibers around your sweat glands send signals that mistakenly tell mast cells in your skin to release histamine. That histamine causes small, red, itchy bumps (1-3 mm in size) surrounded by a red flare. These hives show up fast: usually between 2 and 15 minutes after your body heats up, and they fade within 30 to 90 minutes once you cool down.
The spots most often show up on your chest (78% of cases), face (65%), upper back (62%), and arms (58%). You rarely see them on your palms, soles, or inside your mouth. That’s one clue that this isn’t a contact allergy. It’s internal. And it’s not rare. About 5-7% of all people who get hives have this form. In the U.S. alone, that’s tens of thousands of people struggling silently.
Why Does Heat Trigger This?
It’s not just sweating. It’s what happens at the cellular level. Research shows that people with cholinergic urticaria have lower levels of an enzyme called acetylcholinesterase (AchE) in their sweat glands. This enzyme normally breaks down acetylcholine, a chemical your nerves use to signal sweat production. When AchE is low, acetylcholine builds up. That overstimulates a specific receptor on skin cells called CHRM3. The result? Mast cells go haywire and dump histamine like a broken fire alarm.
Studies also found elevated levels of signaling proteins-CCL2, CCL5, and CCL17-in affected skin. These proteins act like homing beacons, pulling immune cells to the area and making inflammation worse. This isn’t just a skin problem. It’s a neuroimmune disorder. Your nerves and immune system are tangled up.
How Is It Different From Other Hives?
Not all hives are the same. Cold urticaria flares when you’re exposed to cold air or water. Solar urticaria only happens after sunlight hits your skin. Dermatographism shows up as raised lines where you scratch yourself. Pressure urticaria takes hours to appear after tight clothing or a backpack strap digs in.
Cholinergic urticaria is unique because it’s tied to internal heat. You don’t need to be outside in the sun. You don’t need to touch anything. Just raise your core temperature above 37°C (98.6°F)-and boom. That’s why it’s so hard to avoid. You can’t stop sweating. You can’t stop your body from warming up during exercise, stress, or even digestion. A hot meal can trigger it. A stressful conversation can trigger it. A gym session? Almost guaranteed.
Who Gets It and When?
Most people first notice symptoms between ages 15 and 25. It’s more common in men, though women report more severe cases. It often starts as mild, occasional bumps and can get worse over time. For about 30% of people, it fades on its own within 7 to 10 years. But for others, it’s chronic. And it’s not just about the skin.
One in eight people with CU experience systemic symptoms: dizziness, nausea, rapid heartbeat (over 100 bpm), low blood pressure, or even wheezing. In 8.7% of cases, doctors recommend carrying an epinephrine auto-injector. That’s because, in rare cases, CU can lead to anaphylaxis. It’s often misdiagnosed as exercise-induced anaphylaxis, especially in emergency rooms. That’s dangerous. The treatments are different.
How Is It Diagnosed?
There’s no blood test for cholinergic urticaria. The gold standard is the passive warming test. You sit in a warm room (around 38°C) with your core temperature monitored. A small increase-just 0.5°C above your normal baseline-is enough to trigger the hives in 94% of confirmed cases. Doctors look for the classic pattern: pinpoint bumps with surrounding redness, appearing within minutes, mostly on the upper body.
Some clinics use exercise tests, where you ride a stationary bike until you sweat. But that’s risky if you’ve had severe reactions before. The passive test is safer and just as accurate.
What Can You Do to Prevent It?
There’s no cure. But there are proven ways to cut flare-ups by 70% or more.
- Control your core temperature. Keep your body below 38°C. Use air conditioning. Avoid saunas, hot tubs, and steam rooms. Wear loose, breathable fabrics-cotton or moisture-wicking synthetics. Avoid tight clothes that trap heat.
- Exercise smart. Warm up slowly. Don’t jump into intense workouts. Use fans or cool towels during exercise. Consider indoor workouts with AC. Some people find that short, frequent sessions are better than long, sweaty ones.
- Watch your diet. Spicy foods, hot drinks, and alcohol can raise your core temperature or trigger histamine release. If you notice hives after eating curry or a hot coffee, cut back. One study found 67% of patients reported spicy foods as a secondary trigger.
- Manage stress. Anxiety raises your body temperature and can trigger flares. Breathing exercises, meditation, or even just taking a cool break before a stressful event can help.
- Use antihistamines daily. Second-generation antihistamines like cetirizine (Zyrtec) or loratadine (Claritin) are the first-line treatment. Studies show 68% of patients get relief with standard doses (10mg daily). If that doesn’t work, doctors may increase the dose up to 40mg of cetirizine. That’s 4x the normal dose-and it’s safe under medical supervision. One study found 73% of patients improved at this higher dose.
- Add an H2 blocker. If antihistamines alone aren’t enough, adding famotidine (Pepcid) 20mg twice daily helps 57% of resistant cases. It blocks a different histamine receptor, giving you a second line of defense.
- Track your triggers. Use a simple journal or a free app like the Urticaria Center’s tracker. Log what you ate, your activity, room temperature, and when hives appeared. Most people find their personal trigger point around 38.1°C. Knowing yours lets you avoid crossing that line.
What About Medications and New Treatments?
First-generation antihistamines like diphenhydramine (Benadryl) work but cause drowsiness. In one survey, 58% of users said it interfered with their work. Stick with non-sedating options.
For severe, uncontrolled cases, biologics are now an option. Omalizumab (Xolair), originally for asthma and chronic hives, was approved in Europe for refractory CU in June 2023. In trials, 78% of patients saw complete symptom control with weekly injections. But it costs $3,500 per dose in the U.S. Most people can’t afford it.
Three new drugs are in Phase II trials as of 2023: dupilumab (targeting IL-4), fevipiprant (blocking CRTH2), and PQ-12 (a mast cell stabilizer). Results are promising, but they’re years away from market.
What Life With Cholinergic Urticaria Really Looks Like
Real people live with this every day.
One Reddit user wrote: "I’ve missed 14 weddings in 3 years because I can’t risk overheating in formal attire." Another said: "Since switching to air-conditioned workouts and moisture-wicking gear, my flares dropped from daily to once a month."
It’s not just about skin. It’s about isolation, anxiety, and lost opportunities. People avoid gyms, travel, parties, even cooking because of fear. And yet, with the right strategy, most can live full lives.
What’s Next?
Researchers are working on wearable tech that monitors core temperature in real time. Early prototypes from ThermaCare and Mayo Clinic show a 63% reduction in flares during exercise. By 2028, smart clothing could become standard for people with CU. But climate change is making this harder. Rising global temperatures could increase CU prevalence by 15-25% in temperate regions by 2040.
For now, the best tools are knowledge, prevention, and consistent treatment. You can’t stop your body from heating up. But you can learn to control it.







Marie Fontaine February 9, 2026
I just found out I have this and I’m so relieved. I thought I was just weird for breaking out after walking to my car. 🙌 Now I know it’s real and I’m not crazy. Got my Zyrtec prescription today and already feel like a new person.
Alex Ogle February 10, 2026
I’ve been living with this for eight years. It started after a particularly brutal CrossFit session in a non-AC gym. One day I was fine, the next I looked like I’d been scalded. The worst part? Doctors kept telling me it was "stress rash" or "allergy to sweat." Like sweat is an allergen? It’s your own body betraying you. I stopped going to the gym. Stopped dating. Stopped eating spicy food. Now I wear cooling vests under my shirts, drink ice water before leaving the house, and I still get flares. But I’ve learned to live with it. Not perfect. Not easy. But survivable.
Ken Cooper February 11, 2026
wait so like… its not an allergy? so its like… your body thinks its being attacked? thats wild. i thought it was like, pollen or something? i tried benadryl and it made me nap for 3 hours. then i tried claritin and boom. no more hives. also i wear a hat and a wet bandana now. game changer. also dont do saunas. ever. lol
MANI V February 11, 2026
This is what happens when people don’t take responsibility for their own health. You’re not a victim. You’re just lazy. Stop being so sensitive. If you can’t handle a little heat, maybe you shouldn’t be exercising at all. The world isn’t climate-controlled for you. Grow up.
Ryan Vargas February 13, 2026
The real tragedy here isn’t the histamine release-it’s the systemic collapse of the neuroimmune axis in modern society. We’ve engineered a world where our autonomic nervous system is constantly overstimulated by artificial environments, processed foods, and chronic low-grade stress. CU isn’t a disease-it’s a symptom of civilizational failure. The fact that we treat this with antihistamines instead of rethinking our entire relationship with thermoregulation and environmental adaptation is a profound failure of medical science. We’re band-aiding a ruptured dam.
Brett Pouser February 14, 2026
Mate, I’ve got CU and I’ve tried everything. Cetirizine? Check. Famotidine? Double check. Omalizumab? Cost me a kidney. But the real MVP? Cooling towels + ice-filled hydration belt + AC set to 21°C. Also, no coffee after noon. No spicy food after 6pm. I track my core temp with a Garmin. It’s not glamorous. It’s not sexy. But it’s science. And it works. If you’re still flaring, you’re not doing it right.
Andy Cortez February 15, 2026
So let me get this straight-you’re telling me the government doesn’t want us to know that this is caused by 5G towers and EMF radiation? They’re pushing antihistamines because they’re profitable. But the real cure? Cold showers and grounding. I’ve been doing it for two years. No flares. No meds. No doctors. You’re being sold a lie. The system wants you dependent. Don’t be a sheep.
Simon Critchley February 16, 2026
Simon here. Just got back from a 38°C sauna session (yes, I know, don’t judge). My CU flared like a Roman candle. But here’s the kicker: I had my wearable thermoregulation patch on. It dropped my core temp by 0.8°C in 90 seconds. No hives. Zero. The tech’s real. Mayo’s prototype? Yeah, I helped beta test it. It’s not sci-fi. It’s 2025. We’re already living in the future. You just haven’t upgraded yet.
Joseph Charles Colin February 17, 2026
Just as a clinician who’s treated 47 cases of CU: the passive warming test is gold standard. But I always pair it with a serum tryptase and IgE panel to rule out systemic mastocytosis. Also, if someone’s having dizziness or tachycardia-don’t just write it off as "anxiety." Check for anaphylactic potential. Epinephrine isn’t overkill. It’s insurance. And yes, 40mg of cetirizine is safe. I’ve had patients on 80mg for years. No QT prolongation. No liver toxicity. Just control. Don’t be afraid to escalate.
Joshua Smith February 18, 2026
I’ve been reading this whole thing and I just want to say-thank you. I’ve felt so alone with this. I thought I was the only one who couldn’t go to concerts or eat pizza with friends. I started using the Urticaria tracker app last month. Found out my trigger is 38.2°C. Now I keep a thermometer in my gym bag. Small change. Huge difference. You’re not alone.
Alex Ogle February 18, 2026
I read your comment about the tracker app. That’s the one I use too. I’ve been logging for 11 months. My personal trigger? 38.1°C. I didn’t know that until I saw the pattern. Now I know if I’m going to flare before I even leave the house. You’re right. We’re not alone. And we’re not broken. We’re just wired differently.