Blood Thinner Head Injury Risk Assessment
Assessment Criteria
Select all that apply after your head injury
Results
Please select the assessment criteria and click Analyze to see your results
When you’re on blood thinners, even a small bump on the head can feel terrifying. You might think, It’s just a little fall - but that’s exactly when things can turn dangerous. Blood thinners, whether they’re warfarin, rivaroxaban, apixaban, or aspirin, stop your blood from clotting the way it should. That’s good for preventing strokes or clots, but it’s risky when your head takes a hit. A minor head injury in someone on these meds can lead to bleeding inside the skull - and that bleeding can grow quietly, without warning, over hours or even days.
Why Even a Minor Head Injury Is a Big Deal on Blood Thinners
Most people don’t realize how much more likely they are to bleed inside the brain after a head injury if they’re on anticoagulants. Studies show the risk is 2 to 3 times higher than for someone not taking blood thinners. This isn’t just theory - it’s backed by emergency room data from across the U.S. About 1 in 10 people who show up at the ER with a head injury are on these medications. And among them, a surprising number end up with a dangerous bleed, even if they seem fine at first.
Here’s the scary part: you might feel okay right after the injury. No dizziness. No nausea. No confusion. But bleeding can start slowly. It can take hours - sometimes up to 72 hours - before symptoms show up. By then, the pressure inside your skull may have built up enough to cause brain damage or even death.
That’s why guidelines from the American College of Emergency Physicians (ACEP) and the Washington State Department of Health say the same thing: if you’re on blood thinners and you hit your head, get a CT scan immediately. Don’t wait. Don’t hope it’ll pass. Don’t rely on how you feel. The scan is the only way to know for sure.
What Counts as a Head Injury That Needs a Scan?
You don’t need to be knocked out or thrown across the room. Even a simple fall on the sidewalk, bumping your head on a cabinet, or slipping in the shower can be enough. Here’s what triggers the need for a CT scan if you’re on blood thinners:
- Any loss of consciousness - even for a few seconds
- Feeling confused, dazed, or disoriented after the injury
- Memory loss around the time of the injury
- Any visible injury to your head or neck - cuts, bruises, swelling
- A fall from standing height or higher
- Being hit by something heavy - a falling object, a door, a car door
- Being 65 or older - age increases bleeding risk, even with minor trauma
Some people think, But I didn’t lose consciousness - so I’m fine. That’s a dangerous assumption. A 2024 study showed that many patients with delayed bleeding never lost consciousness at all. They just felt a little off. That’s enough reason to get scanned.
What Happens During the CT Scan?
The scan itself is quick - usually under 10 minutes. You lie on a table that slides into a big ring-shaped machine. It takes pictures of your brain using X-rays, but no radiation is left behind. The key is using the right settings. Emergency departments should use bone-algorithm images (0.5 mm to 1.25 mm slices) to catch tiny skull fractures that might be missed otherwise. These fractures can be hidden causes of bleeding.
Before the scan, you’ll likely get a blood test. They’ll check your INR (for warfarin users) or other clotting markers to see how thin your blood is. This helps doctors decide if you need treatment to reverse the blood thinner right away. If your INR is above 3.5, the risk of bleeding skyrockets.
And here’s something many people don’t know: if your CT scan comes back normal, you’re not necessarily in the clear. That’s why observation matters.

Why Observation After a Normal Scan Is Critical
Even if the first CT shows no bleeding, you still need to be watched. Why? Because bleeding can start later. About 0.5% to 1% of people on blood thinners develop a delayed bleed - sometimes 24 to 48 hours after the injury. That’s why hospitals like Johns Hopkins and the University of Texas recommend staying for at least 6 to 23 hours after the injury, even with a normal scan.
Discharge criteria are strict. You can only go home if:
- Your CT scan is completely normal
- You’ve been monitored for at least 6 hours with no change in mental status
- Your INR is below 3.5 (if you’re on warfarin)
- You have no other injuries (like broken ribs or internal bleeding)
- You have someone at home who can watch you for the next 24 hours
If any of those conditions aren’t met, you stay. And yes - you might get a second CT scan 6 hours later, even if you feel fine. It’s not overkill. It’s precaution.
What Not to Do After a Head Injury on Blood Thinners
There are three big mistakes people make:
- Stopping your blood thinner on your own. Some people think, If it caused bleeding, I’ll just stop taking it. But stopping anticoagulants suddenly can trigger a stroke or clot in your lungs or legs. One patient in a Texas case study stopped rivaroxaban after a negative CT - and had a stroke three days later. That’s why reversal should only happen under a doctor’s supervision.
- Waiting to see if symptoms get worse. By the time you’re vomiting, confused, or having trouble speaking, it’s often too late. Don’t wait. Get scanned now.
- Assuming the Canadian CT Head Rule applies to you. That rule is great for healthy people without blood thinners. But it was never tested on people on anticoagulants. In fact, the doctor who created it says applying it to you could miss up to 15% of dangerous bleeds.
What Happens If Bleeding Is Found?
If the CT shows bleeding, doctors have tools to act fast. For warfarin users, they might give vitamin K or a special blood product called PCC (prothrombin complex concentrate) to reverse the effect. For DOACs like apixaban or rivaroxaban, they can use drugs like Idarucizumab (Praxbind) - a targeted antidote that works in minutes.
Not everyone needs surgery. Sometimes, small bleeds are watched closely with repeat scans and kept under control. But if the bleed is growing or putting pressure on the brain, neurosurgeons may need to remove the blood or drill a hole to relieve pressure.
The goal isn’t just to stop the bleeding - it’s to do it before it causes permanent damage. That’s why speed matters. Emergency rooms are supposed to get anticoagulated patients to the CT scanner in under 30 minutes. But studies show they often wait 22 minutes longer than they should. If you’re on blood thinners and you hit your head, insist on immediate imaging.

What to Do After You’re Discharged
If you’re cleared to go home, make sure you have a plan. Someone needs to stay with you for at least 24 hours. Watch for these warning signs:
- Worsening headache
- Repeated vomiting
- Confusion, slurred speech, or trouble understanding
- Weakness or numbness in an arm or leg
- Drowsiness or difficulty waking up
- Seizures
If any of these happen, go to the ER immediately - don’t wait. Call 911. Don’t drive yourself.
Also, don’t restart your blood thinner without talking to your doctor. They’ll weigh the risk of another bleed against the risk of a clot. That’s a decision that needs careful thought - not a rushed call to your pharmacy.
The Bigger Picture: Why This Is Getting Worse
This isn’t a rare problem. It’s growing fast. From 2015 to 2022, prescriptions for blood thinners among Medicare patients jumped 47%. By 2030, over 12 million Americans will be on them. Most are older adults who fell at home - and many are on multiple medications that increase fall risk.
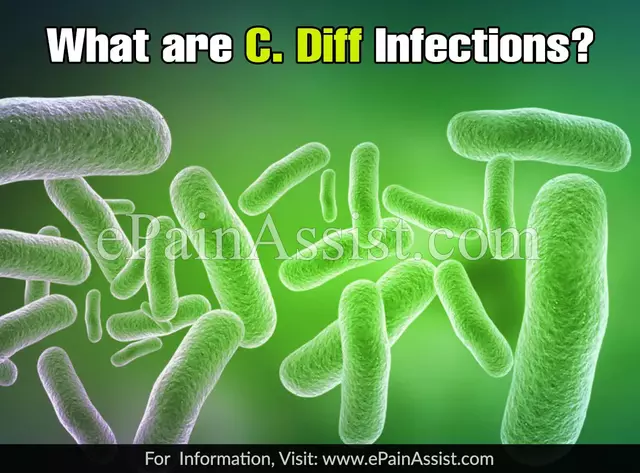
Hospitals are starting to respond. The CDC’s STEADI program now helps doctors assess fall risk and whether blood thinners are still the right choice. Some places are testing blood tests that detect brain injury proteins - like UCH-L1 and GFAP - to avoid unnecessary CT scans. But those tests aren’t ready for routine use yet.
For now, the rule is simple: if you’re on blood thinners and you hit your head, get a CT scan - no exceptions. It’s the only way to be sure you’re safe.
Do I need a CT scan if I only bumped my head and feel fine?
Yes. Even if you feel fine, a minor bump can cause bleeding inside the skull that grows slowly. People on blood thinners have a 2 to 3 times higher risk of bleeding after head trauma. Waiting for symptoms to appear can be dangerous. A CT scan is the only way to rule out bleeding early.
Can I wait a few hours to see if I get worse before getting scanned?
No. Delaying a CT scan increases the risk of serious brain injury. Bleeding can start within minutes and grow over hours. Emergency guidelines recommend immediate imaging for anyone on blood thinners with head trauma - even if they seem okay. Waiting can cost you time, and time can cost you your brain.
What if my CT scan is normal? Can I stop taking my blood thinner?
No. Stopping your blood thinner without medical advice can cause a stroke or dangerous clot. A normal CT means no bleeding was found - not that you should stop your medication. Only your doctor can decide whether to pause, adjust, or restart your anticoagulant based on your overall health and risk factors.
Are there alternatives to a CT scan for checking brain bleeding?
Currently, no. While new blood tests that detect brain injury proteins (like UCH-L1 and GFAP) are being studied, they’re not yet reliable enough to replace CT scans in anticoagulated patients. MRI can detect some bleeds but takes longer and isn’t practical in emergencies. Non-contrast head CT remains the gold standard for fast, accurate diagnosis.
Why can’t I rely on the Canadian CT Head Rule if I’m on blood thinners?
The Canadian CT Head Rule was designed for people not on blood thinners. It was never tested in this group. Studies show that using it on anticoagulated patients could miss up to 15% of serious brain bleeds. That’s why emergency guidelines specifically exclude anticoagulated patients from using this rule. Always assume you need a CT scan if you’re on blood thinners and have head trauma.
What to Do Next
If you’re on blood thinners and haven’t talked to your doctor about head injury risks, make that your next step. Ask: What should I do if I fall or hit my head? Get a written plan. Know which hospital to go to. Tell family members what signs to watch for.
And if you’ve already had a head injury while on blood thinners - even if you were cleared - talk to your doctor about fall prevention. Are your shoes too slippery? Is your home cluttered? Could your medications be making you dizzy? Reducing your risk of falling is just as important as knowing what to do after you fall.






Hilary Miller January 22, 2026
I hit my head last month and just shrugged it off. Thank god I didn't. This post saved my life.
Margaret Khaemba January 23, 2026
My grandma’s on warfarin and she’s always tripping over the rug. I printed this out and taped it to the fridge. Now she knows: no more 'I’m fine' after falls. <3
Malik Ronquillo January 23, 2026
Why are we making people paranoid over a bump? I bet 90% of these scans are useless. ERs are just cash machines. Stop the fearmongering.
Brenda King January 23, 2026
My dad had a bleed after a fall and they didn't scan him for 4 hours because he 'felt okay'... he's lucky to be here. Please don't wait. I've seen what happens. :(
Daphne Mallari - Tolentino January 24, 2026
The empirical rigor of this exposition is commendable. One must acknowledge the evidentiary weight of the ACEP guidelines and the statistical prevalence of delayed intracranial hemorrhage in anticoagulated cohorts. The data are incontrovertible.
Mike P January 24, 2026
You think this is bad? Wait till you're on blood thinners AND your doctor gives you 12 other pills that make you dizzy. Then you fall in Walmart and they treat you like a walking lawsuit. America is a joke.
Sarvesh CK January 24, 2026
It is fascinating to consider the intersection of medical science and societal aging. With increasing life expectancy and the proliferation of anticoagulant prescriptions, we are confronting a paradigm shift in trauma management. The ethical imperative to prioritize early imaging is not merely clinical-it is philosophical. We must ask: what does it mean to value life in an age where frailty is inevitable? The answer lies not in hesitation, but in vigilance.
Kenji Gaerlan January 26, 2026
I got a CT after i fell and they said nothing. Then i went home and woke up with a headache and my wife called 911. Turns out it was a slow bleed. They had to drill my skull. Dont trust your gut. Trust the machine.
Oren Prettyman January 26, 2026
The notion that a non-contrast CT scan constitutes a definitive diagnostic modality for intracranial hemorrhage in the context of anticoagulant use is, in my professional estimation, an oversimplification bordering on negligence. The literature on delayed hemorrhage-particularly in the context of DOACs-demonstrates a significant false-negative rate. A single scan, even with bone algorithm reconstruction, is insufficient. The standard of care should involve serial imaging, mandatory observation windows, and mandatory coagulation profile reassessment at 6, 12, and 24 hours. To suggest otherwise is to endanger public health.
Ryan Riesterer January 27, 2026
The sensitivity of bone-window CT at 0.5mm slice thickness for detecting subtle fractures is well-documented in radiology journals. However, the clinical utility of observing asymptomatic patients post-normal-CT remains contentious. The 0.5–1% delayed bleed rate is statistically significant but operationally challenging in resource-constrained EDs. Still, the risk-benefit calculus favors observation.
Akriti Jain January 28, 2026
They don't want you to know this... but CT scans are actually just a cover for Big Pharma to sell more antidotes. Praxbind costs $4k. Vitamin K is 2 cents. Coincidence? 👀💊