When you pick up a prescription, do you notice the label? Most people don’t. But what if that label-whether it says generic or a well-known brand name-could change how you feel, how well you respond to the medicine, or even whether you take it at all? It sounds strange. After all, the pills are chemically identical. Yet decades of research show that simply knowing a drug is labeled "generic" can make people feel worse, take less of it, or stop taking it entirely-even when the medicine works just as well.
Identical Pills, Different Results
In 2016, researchers at the University of Auckland ran a simple but powerful experiment. They gave 87 students headache pills. Half got ibuprofen. The other half got sugar pills-placebos. But here’s the twist: each pill was labeled either "brand-name" or "generic." The results? People who took the brand-name placebo reported nearly the same pain relief as those who took real ibuprofen. But those who got the generic-labeled placebo? Their pain barely improved. The placebo effect didn’t work when the label said "generic." Even more striking: 63% of people believed the brand-name placebo helped their headache. Only 42% of those with the generic-labeled placebo said the same. And here’s the kicker-the pills were exactly the same in every way except the label.
Why Does the Label Matter?
It’s not about chemistry. It’s about psychology. When you see "generic," your brain often assumes "less effective," "cheaper," "inferior." That’s not based on science. It’s based on perception. And that perception triggers real physical reactions.
This is called the labeling effect. It’s not a myth. It’s measurable. In a 2019 study with 72 participants, researchers gave everyone identical placebo pills. One group was told they were brand-name. The other, generic. After seven days:
- 54% of the generic-labeled group stopped taking the pills before the study ended. Only 33% of the brand-name group did.
- Those with the generic label reported 1.2 points higher pain levels on a 10-point scale.
- 28% of the generic group took extra pills they weren’t prescribed. Only 14% of the brand-name group did.
These aren’t small differences. They’re clinically significant. And they happen even when patients are fully informed the pills are placebos. The label alone changes behavior.
Real-World Consequences
Over 90% of prescriptions filled in the U.S. are for generic drugs. They save patients and the healthcare system billions each year. But if people stop taking them because they think they don’t work, those savings vanish.
For chronic conditions like high blood pressure, diabetes, or depression, adherence is everything. The World Health Organization estimates only about half of people stick to their medication long-term. When the label says "generic," that number drops even further.
A 2022 survey of pharmacists found that 63% had been asked directly by patients: "Is this really the same as the brand?" Many patients refused to take the generic. Others switched back to the brand-despite paying three to five times more.

Who’s Most Affected?
The labeling effect doesn’t hit everyone equally. People with lower health literacy-those who struggle to understand medical terms or instructions-are far more likely to believe generics are inferior. In the 2019 study, 67% of low-literacy patients stopped taking generic-labeled pills. Only 41% of high-literacy patients did.
Older adults, non-native English speakers, and those with anxiety disorders are also more vulnerable. If you’re already worried about your health, seeing "generic" on the bottle can feel like a red flag-even if there’s no reason to be.
More Than Just Perception: Dangerous Label Discrepancies
There’s another layer to this problem. It’s not just what patients think-it’s what the labels actually say.
A 2020 study analyzed 31 generic drugs and found that 100% of them had differences in their labeling compared to the original brand-name version. Four of them had discrepancies that could lead to life-threatening mistakes. Eleven others had potential for serious harm. Nearly half had changes that could seriously affect how the drug was used.
Why? Because generic manufacturers aren’t required to match the exact wording of the original label. They can leave out warnings, change dosing instructions, or simplify language. For a patient reading the label carefully, this creates confusion. For a doctor prescribing it, it creates risk.
What’s Being Done?
Health agencies know this is a problem. The FDA launched the "It’s the Same Medicine" campaign in 2020. It showed real patients saying: "I thought generics were weaker. Then I tried them. They worked just as well." The results? A 28% drop in patient concerns across 12 healthcare systems in just six months.
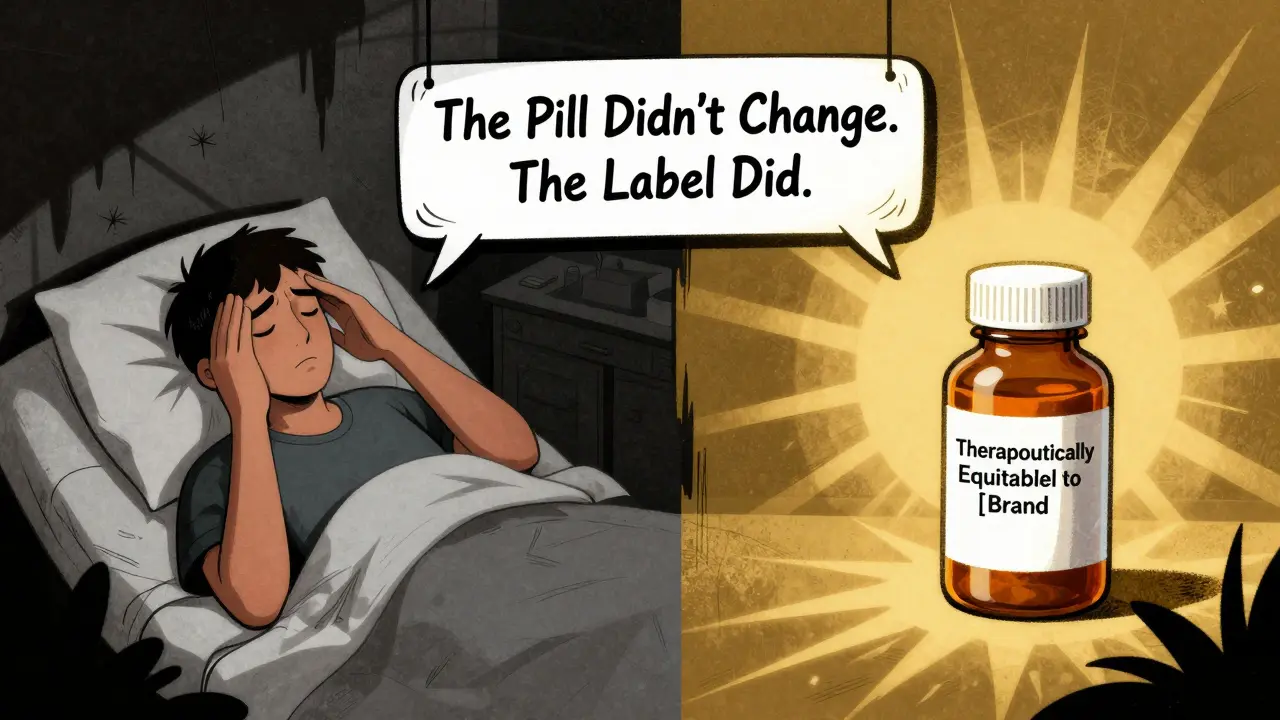
In 2023, a trial tested a simple fix: adding "Therapeutically equivalent to [Brand Name]" to generic labels. Discontinuation rates dropped from 52% to 37%. A small change. A big difference.
Now, the Generic Pharmaceutical Association is spending $50 million on education. The FDA is drafting new guidance to standardize how generics are labeled. The goal? Make it clear: same active ingredient, same effect, same safety.
Why This Matters for Your Health
If you’re on a generic drug and you feel like it’s not working, ask yourself: Is it the medicine-or the label?
Many people switch back to brand-name drugs out of fear. But they’re paying more for the same effect. And sometimes, they’re risking their health by stopping treatment altogether.
On the flip side, if you’re a doctor or pharmacist, don’t assume patients understand the difference. Don’t just hand them a pill and say, "It’s generic." Explain it. Show them the science. Tell them: "This is the exact same active ingredient. It’s not cheaper because it’s worse. It’s cheaper because we don’t spend millions on ads." And if you’re a patient: don’t let a label decide your health. Ask questions. Check the active ingredient. Talk to your pharmacist. You deserve to take the best medicine for you-without fear.
What’s Next?
Experts predict that within five years, high-risk medications-like blood thinners, seizure drugs, or insulin-will have stricter labeling rules. The goal? No more confusion. No more assumptions. Just clear, consistent information.
But until then, the burden falls on us. Patients. Providers. Pharmacies. We have to break the myth that "generic" means "less." Because in reality, it just means "affordable." And that’s something worth fighting for.
Are generic drugs really the same as brand-name drugs?
Yes. By law, generic drugs must contain the same active ingredient, in the same strength, and work the same way as the brand-name version. The FDA requires them to be bioequivalent-meaning they deliver the same amount of medicine into your bloodstream at the same rate. The only differences are in inactive ingredients (like fillers or dyes), packaging, and price. They’re not "copies." They’re legally required to be identical in how they work.
Why do some people feel worse on generic drugs?
It’s rarely because the medicine doesn’t work. More often, it’s because of the labeling effect. If you believe a generic is inferior, your brain can trigger real physical symptoms-like increased pain, anxiety, or nausea-simply because of what the label says. Studies show this happens even when the pill is a placebo. The mind is powerful. And labels shape expectations.
Can generic labels be misleading?
Yes. While the active ingredient must match, the rest of the label doesn’t have to. Some generic labels omit warnings, simplify dosing instructions, or use different formatting than the brand-name version. A 2020 study found that 12.9% of generic labels had discrepancies that could cause life-threatening errors. This isn’t common-but it’s real. Always check the active ingredient and talk to your pharmacist if something feels off.
Does the labeling effect apply to all medications?
It’s strongest for conditions where psychological factors play a big role-like pain, anxiety, depression, and insomnia. These are conditions where the placebo effect is known to help. For antibiotics or insulin, where the effect is purely biological, the labeling effect is weaker. But even then, adherence still drops when patients believe generics are less effective.
How can I tell if a generic is right for me?
Start by checking the active ingredient on the label. If it matches your brand-name drug exactly, it’s the same medicine. Ask your pharmacist: "Is this approved as bioequivalent?" If they say yes, trust it. If you’ve had a bad experience, don’t assume it’s the drug. Talk to your doctor. Sometimes, switching to a different generic manufacturer helps-because inactive ingredients vary. But don’t stop taking it because of the label.