When you're on a blood thinner, the goal isn't to stop your blood from clotting entirely-it's to keep it from clotting too much. But that fine line is where things get dangerous. Every year, 1 in 50 people taking anticoagulants end up in the hospital because of uncontrolled bleeding. It’s not rare. It’s predictable. And it’s often preventable.
Why Blood Thinners Are Necessary-and Risky
Anticoagulants save lives. They prevent strokes in people with atrial fibrillation, stop deadly clots in the legs and lungs, and protect those with mechanical heart valves. But every time you take one, you’re trading a risk of clotting for a risk of bleeding. That’s the trade-off. And it’s not the same for everyone. Warfarin has been around since the 1950s. It works by blocking vitamin K, which your body needs to make clotting factors. But it’s finicky. Your INR (International Normalized Ratio) has to stay between 2.0 and 3.0 for most people. If it’s too low, you’re at risk for a stroke. Too high, and you could bleed internally without warning. Studies show that if your time in therapeutic range drops below 70%, your risk of major bleeding jumps by 15% for every 10% drop. Newer drugs-called DOACs (direct oral anticoagulants)-like apixaban, rivaroxaban, and dabigatran, were supposed to fix this. They don’t need constant blood tests. They have fewer food interactions. And overall, they cause about 20% less major bleeding than warfarin. Apixaban, in particular, cuts major bleeding risk by 31% compared to warfarin in clinical trials. But they’re not perfect. And they’re not for everyone.Who’s at Highest Risk for Bleeding?
Not everyone on anticoagulants is equally likely to bleed. Certain factors stack the deck against you:- Age over 75: Bleeding risk doubles or triples. Kidneys slow down. Drug levels build up. Even small dosing errors become dangerous.
- Chronic kidney disease: If your creatinine clearance is below 50 mL/min, your bleeding risk doubles. DOACs are cleared through the kidneys. If they can’t flush the drug, it stays in your system too long.
- Combining with aspirin or NSAIDs: Taking ibuprofen, naproxen, or even low-dose aspirin with a blood thinner increases major bleeding by 50-70%. Many people don’t realize they’re doubling their risk.
- History of prior bleeding: If you’ve had a GI bleed or brain bleed before, your chance of another one is much higher.
- Unstable INR: Warfarin users who jump from INR 1.8 to 4.5 in a week are at serious risk. Fluctuations matter more than average numbers.
DOACs vs. Warfarin: Choosing the Right One
It’s not about which drug is better. It’s about which one’s right for you.| Drug | Monitoring Needed? | Renal Dose Adjustment | Reversal Agent | Cost (Monthly, No Insurance) | Best For |
|---|---|---|---|---|---|
| Warfarin | Yes (INR weekly/monthly) | None | 4f-PCC + Vitamin K | $4 | Mechanical heart valves, antiphospholipid syndrome |
| Apixaban | No | Yes (CrCl <25 mL/min) | Andexanet alfa | $550 | Most AFib patients, lower bleeding risk |
| Rivaroxaban | No | Yes (CrCl <50 mL/min) | Andexanet alfa | $550 | Deep vein thrombosis, pulmonary embolism |
| Dabigatran | No | Yes (CrCl <30 mL/min) | Idarucizumab | $550 | AFib patients with normal kidney function |
| Enoxaparin (Lovenox) | Occasional anti-Xa | Yes (CrCl <30 mL/min) | Protamine (partial) | $300 | Acute settings, pregnancy, renal impairment |
DOACs are the default choice for most people today-75% of new prescriptions in the U.S. are for them. But if you have a mechanical mitral valve or antiphospholipid syndrome, warfarin is still the only option. DOACs can actually increase clotting risk in those cases.

How to Prevent Bleeding Before It Happens
Prevention isn’t just about taking your pill correctly. It’s about building a safety net around your treatment.- Get your kidneys checked. Every 3-6 months if you’re on a DOAC. If your creatinine clearance drops below 30 mL/min, your dose needs to change-or you may need to switch back to warfarin.
- Avoid NSAIDs like the plague. Use acetaminophen for pain instead. If you need an anti-inflammatory, talk to your doctor. There’s no safe dose of ibuprofen or naproxen on blood thinners.
- Don’t stop and start your medication. Missing a dose or taking two to make up for it is a common cause of bleeding and clotting. Set phone reminders. Use pill organizers. If you miss a dose, check the specific instructions for your drug-don’t guess.
- Know your reversal agents. If you’re on apixaban or rivaroxaban, your hospital should have andexanet alfa available. If you’re on dabigatran, they need idarucizumab. Ask your doctor: “What’s the plan if I bleed?” If they don’t have an answer, find a new provider.
- Wear a medical alert. A bracelet or necklace that says “On Anticoagulant” could save your life in an emergency. Paramedics won’t know what’s in your system unless you tell them.
What Happens If You Bleed?
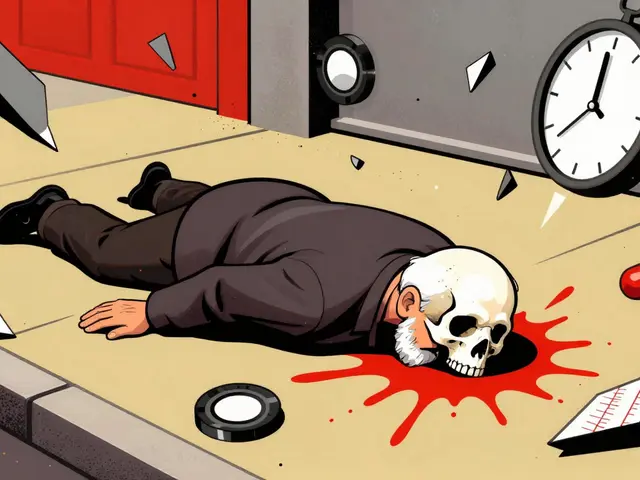
Not all bleeding is an emergency. A small nosebleed or bruise? Usually fine. But if you have:- Head trauma with confusion or vomiting
- Bright red blood in stool or black, tarry stools
- Severe abdominal or back pain
- Sudden weakness or speech trouble
- Uncontrolled bleeding from a cut or wound
Go to the ER immediately. Don’t wait. Time matters.
For warfarin, hospitals use 4f-PCC (four-factor prothrombin complex concentrate) to reverse it in minutes-not hours. Vitamin K helps too, but it takes 8-24 hours to work. For DOACs, reversal agents exist, but they’re expensive. Andexanet alfa costs about $13,000 per dose. That’s why prevention is so much cheaper than treatment.
What About Women and Pregnancy?
Pregnant women on anticoagulants need special care. Warfarin can cause birth defects, so it’s avoided after the first trimester. Low molecular weight heparins like enoxaparin are the standard. They don’t cross the placenta. But they require daily injections.For women with a history of unprovoked blood clots, anticoagulation during pregnancy reduces the risk of recurrence by 75%. Even during procedures like early abortion, many women on anticoagulants lose less than 100 mL of blood-far less than the 500 mL that defines a major hemorrhage. But hemoglobin can still drop below 7 g/dL, so monitoring is essential.
What’s Next for Anticoagulant Safety?
The future is promising. A new drug called ciraparantag is in trials-it could reverse all anticoagulants with one shot. That would be a game-changer. Point-of-care tests for DOACs are also being developed. Imagine a device like a glucose meter that tells you your drug level in minutes. That could cut bleeding events by 15-20%.For now, the best tools we have are knowledge, vigilance, and communication. If you’re on a blood thinner, you’re not just a patient-you’re a partner in your own safety.
Can I take aspirin while on a blood thinner?
No, unless your doctor specifically tells you to. Combining aspirin with anticoagulants increases your risk of major bleeding by 50-70%. Even low-dose aspirin (81 mg) is risky. Use acetaminophen for pain instead. Always check with your provider before adding any new medication, including over-the-counter ones.
Do I need to stop my blood thinner before surgery?
It depends on the procedure and your clotting risk. For minor procedures like dental work, you usually don’t need to stop. For major surgery, your doctor will weigh the risk of bleeding against the risk of a clot. Some DOACs are stopped 24-48 hours before surgery; warfarin may be stopped 5 days out. Never stop on your own. Always follow your provider’s plan.
Can I drink alcohol while on anticoagulants?
Moderate alcohol is usually okay-one drink per day for women, two for men. But heavy drinking can increase bleeding risk and interfere with warfarin metabolism. If you drink regularly, tell your doctor. They may need to check your INR more often. Avoid binge drinking entirely.
What should I do if I fall and hit my head?
Even if you feel fine, go to the ER. Bleeding inside the skull can develop slowly. Symptoms like dizziness, nausea, confusion, or blurred vision may not appear for hours. A CT scan can catch a bleed early. Don’t wait. Your life could depend on it.
Are natural supplements safe with anticoagulants?
Many are not. Garlic, ginkgo, ginger, fish oil, and vitamin E can all increase bleeding risk. Turmeric and green tea may interfere with warfarin. Always tell your doctor what supplements you take-even if you think they’re “natural” or “harmless.”





Erin Nemo December 2, 2025
Just started apixaban last month and I already got a bracelet. Seriously, if you're on one of these, get the damn bracelet. Paramedics saved my cousin's life because it said 'ON ANTICOAGULANT'-he didn't even know he'd hit his head until they found the bleed.
Suzanne Mollaneda Padin December 3, 2025
Thanks for this. I'm 78 and on warfarin after a stroke. My INR's been stable for 18 months, but I still get nervous every time I have a nosebleed. I never realized how much kidney function matters-I got my CrCl checked last week and it's down to 42. My doc just switched me to a lower dose of apixaban. Feels good to be proactive.
Charlotte Collins December 5, 2025
Let’s be real-DOACs are a cash grab disguised as progress. $550 a month? And you can’t even reverse them without a $13k drug? Warfarin’s been around since WWII and costs four bucks. The system doesn’t care if you bleed-it cares if you keep paying. And don’t even get me started on how they push these drugs while ignoring diet, exercise, and vitamin K balance.
Bonnie Youn December 5, 2025
STOP TAKING NSAIDS LIKE THEY’RE CANDY. I lost my uncle to a GI bleed because he took ibuprofen for his arthritis and didn’t think it mattered. He was on rivaroxaban. He didn’t even know it was dangerous. If you’re reading this and you’re on a blood thinner-go throw out your Advil right now. Use Tylenol. Your body will thank you. And if your doctor says it’s fine? Get a new doctor.
amit kuamr December 7, 2025
Indian healthcare system here. We don’t even have access to reversal agents. My father is on warfarin and we do INR tests at a local lab that charges 200 rupees per test. No one here knows what andexanet alfa is. The real issue isn’t the drug-it’s the lack of infrastructure. People die not because they’re careless but because the system fails them. This post reads like it was written for a US private hospital patient. What about the rest of us?
Amber-Lynn Quinata December 8, 2025
Ugh I just saw someone on Reddit say they take fish oil with apixaban ‘because it’s natural’ 😭 like bro you’re gonna bleed out in your sleep and then we’ll all be reading your obituary like ‘poor guy just wanted healthy omega-3s’ 🤦♀️🥲 I swear people think ‘natural’ means ‘safe’ like it’s a magic word. Turmeric? Ginger? Garlic pills? All blood thinners. Just stop. Your grandma’s kitchen remedies aren’t FDA approved for a reason.
Margaret Stearns December 9, 2025
i got my kidney test done last week and my crcl was 28 so my dr switched me from dabigatran to low dose warfarin. i was scared but now i feel better knowing theyre monitoring me. also i wear my medical alert bracelet every day even to bed. its a little annoying but worth it. thanks for the info.
Scotia Corley December 11, 2025
It is imperative to note that the decision to prescribe anticoagulants must be individualized, taking into account not only renal function and comorbidities, but also socioeconomic factors, medication adherence capacity, and access to monitoring resources. The widespread adoption of DOACs without equitable access to reversal agents constitutes a systemic ethical failure in contemporary clinical practice.