When your immune system is weakened-whether by disease, transplant, or the very drugs meant to help you-taking medication becomes a high-stakes balancing act. For immunocompromised patients, a simple cold can turn dangerous. A minor skin infection might spread fast. Even a vaccine might not work the way it should. This isn’t theoretical. It’s daily reality for millions.
What Does ‘Immunocompromised’ Really Mean?
Being immunocompromised means your body’s defense system isn’t working like it should. You’re not just more likely to get sick-you’re more likely to get seriously sick. The immune system normally fights off viruses, bacteria, and fungi. When it’s suppressed, those invaders move in unchecked. This can happen because of conditions like HIV, leukemia, or lupus. Or because of medications: steroids, biologics, chemotherapy, or drugs taken after an organ transplant.
The key thing to understand: it’s not one-size-fits-all. Someone on low-dose prednisone for a month has a very different risk than someone on a combination of tacrolimus, mycophenolate, and a biologic after a kidney transplant. The level of suppression, the type of drug, and how long you’ve been on it all matter.
The Big Danger: Infections That Don’t Act Like Infections
Most people know the signs of infection: fever, chills, swollen lymph nodes, cough, redness. But for immunocompromised patients, those signs often don’t show up-or they show up late. Corticosteroids like prednisone can mask fever. That’s dangerous. You might have pneumonia, but your temperature is normal. You might have a serious bacterial infection, but you don’t feel particularly unwell.
That’s why infections in this group are called "atypical." They don’t follow the usual playbook. A skin rash might be a fungal infection. A headache could be meningitis. A cough might not be a cold-it could be Pneumocystis jirovecii pneumonia, a rare lung infection that only hits people with severely weakened immunity.
Studies show people on corticosteroids (especially above 20mg of prednisone daily for more than two weeks) have a 60% higher chance of getting an infection compared to those not on these drugs. And it’s not just common bugs. Opportunistic infections-ones that rarely hurt healthy people-are a real threat. These include:
- Herpes zoster (shingles) reactivation
- Cytomegalovirus (CMV) viremia
- Progressive multifocal leukoencephalopathy (PML) from JC virus
- Nocardia and Aspergillus infections
- Hepatitis B or C flare-ups
Biologics-drugs like Humira, Enbrel, or Remicade-carry the highest infection risk of all. They target specific parts of the immune system, but that precision comes at a cost. Many patients on these drugs report hospitalizations for infections, especially shingles or pneumonia.
How Different Drugs Affect Your Risk
Not all immunosuppressants are the same. Each class has its own profile:
Corticosteroids (Prednisone, Dexamethasone)
These are the most common. Used for everything from asthma to rheumatoid arthritis. But they’re also the most likely to cause trouble. Risk goes up sharply at doses over 20mg per day. Even short courses-like for a COPD flare-can raise infection risk if you’re already vulnerable. The longer you’re on them, the worse it gets.
Conventional DMARDs (Methotrexate, Leflunomide, Azathioprine)
Methotrexate is the go-to for many autoimmune diseases. About 70% of patients say it controls their symptoms well. But nearly half quit within a year because of side effects: nausea, fatigue, mouth sores, hair thinning. It also lowers white blood cells. That’s why monthly blood tests are standard-watching for drops in counts before infection hits.
Azathioprine (Imuran) is tougher on the bone marrow. It can cause severe leukopenia (low white blood cells), which opens the door to serious bacterial infections. It’s also linked to hepatitis reactivation and PML.
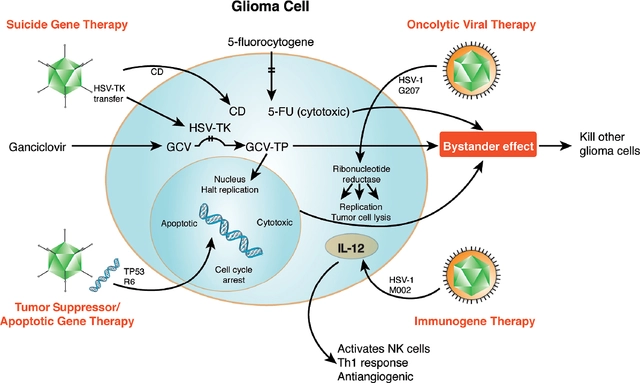
Biologics (TNF inhibitors, IL inhibitors)
These are powerful. They can turn a life of pain into a life of function. But they come with a price. Studies show biologics are significantly more likely to cause infections than older DMARDs. One patient on Reddit shared how they got shingles on Humira-despite being vaccinated. Another developed a lung infection that required ICU care.
Calcineurin Inhibitors (Cyclosporine, Tacrolimus)
These are common after transplants. Tacrolimus is called "life-changing" by many transplant recipients. But it’s also tied to viral complications: Epstein-Barr virus (which can cause lymphoma), hepatitis C, and BK virus (which damages kidneys). Blood levels must be checked often. Too high? Toxic. Too low? Rejection.
Chemotherapy Drugs
Drugs like cyclophosphamide or paclitaxel aren’t just for cancer. They’re sometimes used for severe autoimmune disease. These drugs wipe out rapidly dividing cells-including immune cells. The result? A deep, wide suppression. Infection risk is high, and recovery is slow.
Combining Drugs = Higher Risk
Doctors often combine medications to get better control. But that’s where things get risky. The combination of steroids and another immunosuppressant doesn’t just add risk-it multiplies it. A patient on methotrexate and prednisone has a much higher chance of infection than someone on either drug alone. The same goes for biologics plus steroids. The immune system gets hit from multiple angles.
There’s no magic formula for safety. But the rule is simple: the more drugs, the higher the danger. That’s why doctors try to use the lowest effective dose and the fewest number of drugs possible.

What You Can Do to Protect Yourself
Living with immunosuppression doesn’t mean living in fear. It means being smart. Here’s what actually works:
- Wash your hands like your life depends on it. At least 20 seconds. Scrub between fingers, under nails, up to your wrists. Use alcohol-based sanitizer when soap isn’t available.
- Wear a mask in crowded places. Especially during flu season or when there’s a surge in respiratory viruses. Hospitals, public transport, grocery stores-these are high-risk zones.
- Get vaccinated-but know the limits. You need vaccines before starting immunosuppressants if possible. But even after, you need them. Flu shot? Yes. Pneumococcal? Yes. Shingles vaccine (Shingrix)? Yes-if you’re not on active high-dose therapy. Live vaccines (like MMR or nasal flu) are off-limits.
- Watch for subtle signs. A low-grade temperature, unusual fatigue, a new rash, a sore that won’t heal-don’t wait. Call your doctor immediately.
- Protect your skin. Cuts, scrapes, insect bites-clean them right away. Use antibiotic ointment. Avoid gardening or handling soil without gloves. Fungi live in dirt.
- Be extra careful with mosquitoes and ticks. The CDC warns immunocompromised people are at higher risk for diseases like West Nile or Lyme. Use repellent. Wear long sleeves. Check for ticks after being outside.
What About COVID-19? The Surprising Truth
A few years ago, everyone assumed immunosuppressed patients would die from COVID-19. The fear was real. But a 2021 study from Johns Hopkins shattered that assumption. Researchers found that patients on immunosuppressive drugs had outcomes similar to those without them. Why? It’s still being studied. Maybe the drugs helped calm the dangerous overreaction of the immune system-the cytokine storm-that kills some COVID patients.
This doesn’t mean you’re safe. It means your risk isn’t automatic. It depends on your specific condition, your meds, your age, and other health issues. But it does show that blanket assumptions about immunosuppression and infection don’t always hold up. Personalized care matters more than ever.
Monitoring and Testing: Your Lifeline
You can’t manage what you don’t measure. Regular blood tests are non-negotiable.
- Complete Blood Count (CBC): Checks white blood cells, red blood cells, platelets. Methotrexate patients need this monthly at first.
- Liver and Kidney Function Tests: Many drugs stress these organs. Leflunomide and azathioprine can cause liver damage. Tacrolimus affects kidneys.
- Viral Load Tests: For patients on biologics or transplant meds, doctors may check for CMV, EBV, or hepatitis.
If your counts drop, your dose may be lowered-or stopped. That’s not failure. It’s safety.
It’s Not All Bad News
Yes, the risks are real. But so are the benefits. Many patients on immunosuppressants go from being bedridden to hiking, working, playing with grandkids. One transplant recipient said tacrolimus gave them back their life. A woman with rheumatoid arthritis said methotrexate ended her chronic pain.
The goal isn’t to avoid medication. It’s to use it wisely. To know your risks. To act fast when something feels off. To partner with your doctor-not just take orders, but ask questions, track symptoms, and speak up when something doesn’t feel right.
What’s Next? The Future of Safer Treatment
Scientists are working on smarter drugs. JAK inhibitors like Xeljanz target specific immune pathways, hoping to reduce broad suppression. Pharmacogenomics is starting to help predict who will have bad side effects based on their genes. New biomarkers might soon tell us who’s at highest infection risk before they even get sick.
But for now, the tools we have are powerful-and dangerous. The key isn’t waiting for perfect drugs. It’s using the ones we have with care, awareness, and vigilance.
Can I still get vaccinated if I’m immunocompromised?
Yes-but not all vaccines are safe. You should get inactivated vaccines like the flu shot, pneumococcal vaccine, and Shingrix (the non-live shingles vaccine). Live vaccines like MMR, varicella, or the nasal flu spray are dangerous and should be avoided. Always check with your doctor before getting any shot. Timing matters too-some vaccines work best before starting immunosuppressants.
Do immunosuppressants increase cancer risk?
Yes, long-term use of some immunosuppressants raises the risk of certain cancers, especially skin cancer and lymphoma. This is why regular skin checks are critical. Avoid sun exposure, wear sunscreen daily, and get annual dermatology exams. The FDA requires black box warnings on many of these drugs for this reason.
Why do I feel so tired on methotrexate?
Fatigue is one of the most common side effects. It usually hits 24-48 hours after your dose. Taking folic acid daily can help reduce it. Also, avoid alcohol and make sure you’re sleeping well. If fatigue is severe, your doctor may lower your dose or switch you to another drug.
Should I avoid pets if I’m immunocompromised?
No-you don’t need to give up your pets. But be careful. Avoid cleaning litter boxes or bird cages. Wash your hands after petting animals. Don’t let them lick your face or open wounds. Reptiles and exotic pets carry higher infection risks, so avoid them if possible.
What should I do if I develop a fever?
Call your doctor immediately-even if the fever is low-grade. Don’t wait. Don’t take Tylenol and hope it goes away. In immunocompromised patients, fever is a medical emergency until proven otherwise. You may need blood tests, imaging, or even hospitalization to rule out serious infection.
Can I travel while on immunosuppressants?
You can-but plan carefully. Avoid areas with high risk of malaria, dengue, or other vector-borne diseases. Make sure your medications are packed in your carry-on. Bring extra in case of delays. Know where the nearest hospital is at your destination. Carry a letter from your doctor explaining your condition and meds. Avoid raw foods, untreated water, and street vendors.
Final Thought: You’re Not Alone
Managing immunosuppression is hard. It’s exhausting. It’s scary. But you’re not alone. Millions of people walk this path every day. They’re working, parenting, traveling, living full lives-while staying vigilant. The key isn’t perfection. It’s awareness. It’s communication. It’s knowing your body well enough to spot when something’s wrong before it becomes a crisis.
Ask questions. Keep records. Trust your gut. And never ignore a symptom just because you think it’s "probably nothing." In your case, it might not be nothing at all.






Jamie Hooper January 23, 2026
so i got on prednisone for my asthma last year and honestly thought i was gonna die from a sneeze. like i started wearing a mask to the fridge. my cat looked at me like i’d betrayed him. turns out i’m fine. but yeah, i check every little rash now. #scaredbutalive
Husain Atther January 25, 2026
This is a well-researched and thoughtful overview. For many in developing countries, access to regular blood tests or even basic antifungal medications remains a challenge. The emphasis on vigilance and monitoring is crucial, but systemic support is equally vital.
Izzy Hadala January 26, 2026
The assertion regarding COVID-19 outcomes in immunocompromised populations warrants further scrutiny. The referenced Johns Hopkins study, while informative, was observational and did not control for variables such as vaccination status, timing of immunosuppressant initiation, or comorbidities. A meta-analysis from 2023 suggests a 2.3x higher mortality rate in this cohort when unvaccinated. The nuance here is critical.
Vatsal Patel January 27, 2026
Oh wow. So we’re just supposed to be grateful these drugs don’t turn us into piles of ash? Let me guess - next you’ll tell me breathing is optional. I’m on three immunosuppressants and I’ve had three hospitalizations. They call it a ‘balance’. I call it Russian roulette with a prescription pad.
Sharon Biggins January 27, 2026
i just wanted to say… you’re not alone. i’ve been on methotrexate for 5 years. i cry sometimes. but i also hike. and i bake cookies. and i laugh with my kids. it’s hard. but it’s worth it. take folic acid. drink water. and don’t feel guilty for needing rest.
John McGuirk January 28, 2026
you ever wonder if Big Pharma is just selling fear? like… what if the real problem is that we’re all just too clean? no dirt, no germs, no immune system training? i mean… i’ve never had a cold since i started my meds. maybe we’re all just being programmed to be weak?
Michael Camilleri January 30, 2026
people like you think you can just take drugs and live like normal people but you cant. you think its your right to be sick and still go to the grocery store and touch the same cart handles as healthy people. you're a walking biohazard and you dont even know it. stop being so selfish
lorraine england January 31, 2026
I love how you broke down each drug class - so helpful! I just started on Humira and was terrified, but this made me feel way more informed. Also, the handwashing tip? Game changer. I started doing it after every time I open my fridge. My partner thinks I’m weird. I don’t care.
Darren Links January 31, 2026
I’m from the US and I’ve seen this play out. People on Medicaid can’t get monthly blood tests. People without insurance skip doses because the meds cost $3k/month. This article reads like it was written for rich people who can afford to be paranoid. Meanwhile, my cousin died from a simple UTI because she couldn’t get her tacrolimus refilled.
Kevin Waters February 1, 2026
Just wanted to add something practical: if you’re on biologics, keep a symptom journal. I started noting even tiny changes - fatigue timing, skin dryness, joint stiffness - and it helped my rheumatologist catch a low-grade CMV flare before it became serious. Small details matter. Also, folic acid for methotrexate? Non-negotiable. I wish I’d known that sooner.
Kat Peterson February 2, 2026
I’m on 3 meds and I just got my nails done 😍💅 I know I’m not supposed to but… I’m alive and I want to feel beautiful. Also I cried at the salon because the girl asked if I was okay and I said ‘yes’ and then cried harder. We deserve to feel good. 💕
Himanshu Singh February 4, 2026
This is beautiful. The truth is, medicine is a tool, not a promise. We’re not broken. We’re adapting. I used to think my body was failing me. Now I see it’s learning. Every infection, every blood test, every sleepless night - it’s all part of the story. And yours? It’s still being written. 🌱