Bedwetting Risk Calculator
When a child drags the sheets in the middle of the night, most parents instinctively think it’s just a phase. In reality, night‑time wetting-known as Bed-wetting (nocturnal enuresis) is involuntary urination during sleep in children older than five years-is often a sign that the bladder’s control mechanisms aren’t fully in sync. This article pulls apart the physiology, common medical triggers, and everyday factors that tie bladder control to bed‑wetting, giving you a clear roadmap for what to watch, when to act, and how to help your child regain dry nights.
Key Takeaways
- Bladder control develops through a balance of muscle strength, nerve signaling, and hormone regulation.
- Night‑time wetting can stem from primary (developmental) or secondary (medical) causes.
- Common culprits include low antidiuretic hormone, small functional bladder capacity, constipation, and sleep‑cycle disruptions.
- Professional assessment is needed if wetting persists after age 7, appears suddenly, or is accompanied by pain.
- Effective strategies range from fluid‑timing and bathroom routines to enuresis alarms and focused behavioral therapy.
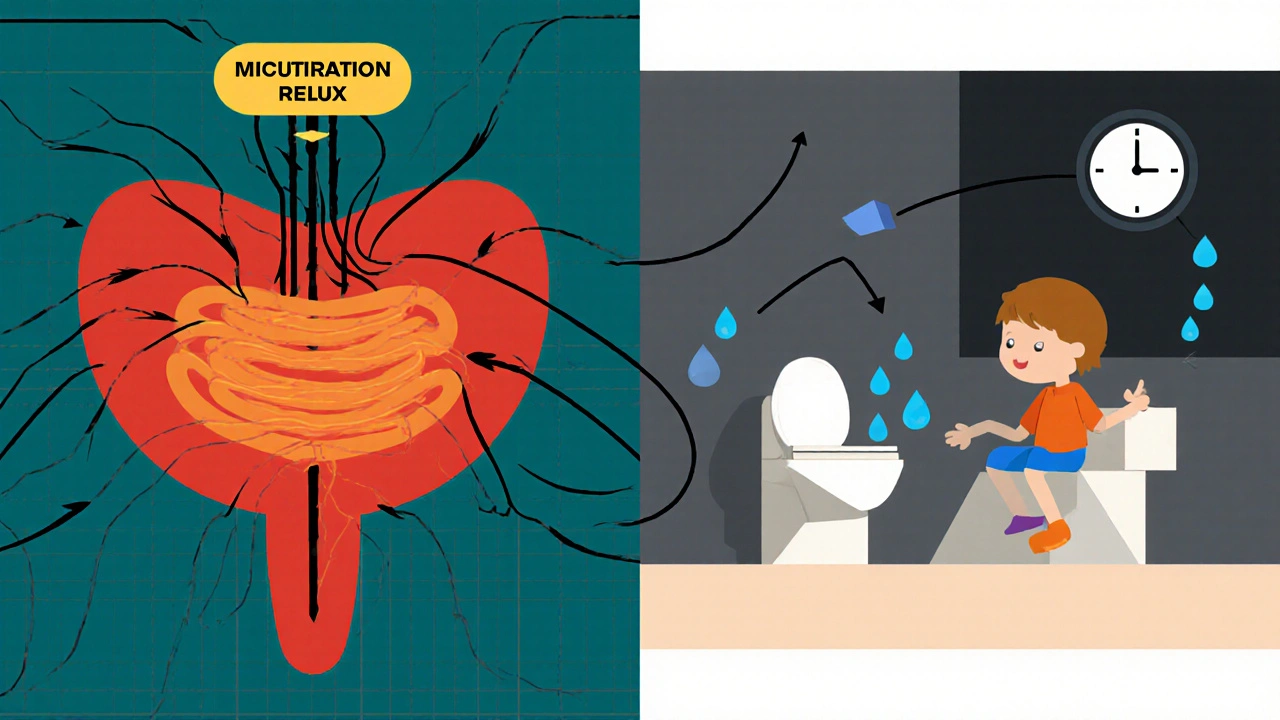
How Bladder Control Develops in Kids
The bladder is more than a stretchy balloon; it’s a coordinated system of muscles, nerves, and hormones. Early on, the Detrusor muscle is the smooth‑muscle layer that contracts to expel urine learns to contract only when the bladder reaches a safe volume. Simultaneously, the brain‑spinal cord pathway, called the micturition reflex a loop that tells the brain when the bladder is full and triggers the urge to void, matures. By age 4‑5, most children can consciously suppress this reflex during the day, but nighttime suppression lags because of different hormonal cues.
Why Children Wet the Bed
Three core reasons explain night‑time wetting:
- Insufficient hormone signal: Antidiuretic hormone (ADH) reduces urine production during sleep typically peaks around 2 a.m. In younger kids, ADH production may be low, leading to excess urine that overwhelms the bladder.
- Limited bladder capacity: Functional bladder capacity the maximum volume the bladder can hold without triggering a strong urge varies by age. A child whose capacity is 100 ml may fill up twice during a typical eight‑hour sleep.
- Sleep‑cycle factors: Deep, non‑REM sleep can blunt the brain’s awareness of bladder signals. A child who stays in deep sleep longer may not wake to use the bathroom even if the bladder is full.
When any of these factors are out of balance, the result is wet sheets.
Medical Conditions That Can Trigger Bed‑Wetting
While many cases are purely developmental, several health issues can suddenly introduce night‑time accidents. Recognising these secondary causes helps parents know when a doctor’s visit is warranted.
| Cause Type | Typical Signs | Suggested Check‑up |
|---|---|---|
| Urinary Tract Infection | Painful urination, fever, foul‑smelling urine | Urine culture and antibiotics if positive |
| Constipation | Hard stools, abdominal bloating, infrequent bowel movements | Stool softeners, dietary fibre increase |
| Diabetes Mellitus | Excessive thirst, frequent daytime urination, weight loss | Blood glucose test, endocrinology referral |
| Neurological Issues | Weakness, spasticity, abnormal gait | Neurological exam, imaging if indicated |
Other red‑flag conditions include spinal cord anomalies, sleep‑apnea, and certain medications that increase urine output. If wetting appears suddenly after a period of dryness, schedule a pediatrician appointment.
Behavioural and Environmental Influences
Even when the physiology is fine, everyday habits can push a child over the edge.
- Fluid timing: Large drinks right before bedtime flood the bladder. Aim for a balanced intake throughout the day and limit caffeine‑containing sodas.
- Bathroom routine: Skipping the nightly potty trip, especially after dinner, reduces the chance the bladder empties fully.
- Stress and anxiety: Emotional upheavals-starting school, a family move, or parental conflict-can heighten nighttime accidents. The brain may prioritize coping over bladder signals.
- Sleep setup: A very warm bedroom or a deep‑sleep‑inducing bedtime story can prolong deep sleep stages, muffling the urge to wake.
Addressing these factors doesn’t require a medical prescription-just attention to daily patterns.
When to Seek Professional Help
Most pediatric guidelines suggest monitoring until age 5‑6. However, reach out to a healthcare provider if any of the following apply:
- Bed‑wetting persists beyond age 7 despite a consistent routine.
- Wetting starts abruptly after months of dryness.
- Wetting is accompanied by pain, blood in urine, or daytime urgency.
- Family history of diabetes, kidney disease, or neurological disorders.
A pediatrician will likely review growth charts, conduct a urinalysis, and ask about bowel habits. In complex cases, referral to a pediatric urologist or gastroenterologist may follow.
Effective Management Strategies
Once medical causes are ruled out, many families find success with a tiered approach.
- Fluid‑timing plan: Encourage hydration earlier in the day, set a “no‑drink” rule after 7 p.m., and offer a small glass of water before bed.
- Scheduled bathroom trips: Have the child sit on the toilet for 5 minutes after dinner and right before lights out, even if they don’t feel the urge.
- Address constipation: Increase fibre, ensure regular daytime bowel movements, and use child‑friendly stool softeners if needed.
- Enuresis alarm: Enuresis alarm a device that detects moisture and wakes the child to use the bathroom has a 70‑80 % success rate after 2-3 months of consistent use.
- Behavioural therapy: Behavioral therapy techniques such as positive reinforcement, reward charts, and relaxation exercises helps reduce anxiety‑related wetting and builds confidence.
In rare cases where the child’s ADH production is markedly low, a pediatrician may prescribe a low‑dose desmopressin tablet, but this is usually a short‑term supplement combined with the behavioural plan.
Putting It All Together
Understanding the tie between bladder control and bed‑wetting gives parents a clear diagnostic lens. Look for physiological signals-hormone levels, bladder capacity, and sleep patterns-while also scanning daily habits and emotional wellbeing. When red‑flag symptoms appear, get a medical review. Otherwise, a structured routine, a supportive environment, and tools like an enuresis alarm can turn wet nights into dry ones.
How old is it normal for a child to still wet the bed?
Most children outgrow nocturnal enuresis by age 5‑6. If wetting continues past age 7, a pediatric evaluation is advisable.
Can a simple potty‑training schedule stop bed‑wetting?
A consistent schedule helps, especially when paired with a bedtime toilet visit, but it may need to be combined with fluid timing and, for many kids, an enuresis alarm for best results.

What role does constipation play in night‑time accidents?
A full colon can press on the bladder, reducing its functional capacity and triggering involuntary leaks. Treating constipation often reduces bed‑wetting frequency.
Are medications like desmopressin safe for children?
Desmopressin is approved for children over 6 years when other methods fail. It should be used under a doctor’s supervision, as misuse can lead to water‑balance issues.
How long does it take for an enuresis alarm to work?
Most families see a noticeable drop in accidents after 2-3 months of nightly use, with full success often reached by 6 months.
Can stress cause a child who was dry to start wetting again?
Yes. Emotional stress can interfere with the brain’s ability to recognize bladder signals during deep sleep, leading to regression.
Is there a link between night‑time wetting and ADHD?
Studies show a higher prevalence of enuresis in children with ADHD, likely due to delayed maturation of the micturition reflex and sleep‑pattern differences.
If you’ve been searching for why your child still struggles with night‑time accidents, the answer often lies in a mix of bladder development, hormone timing, and day‑to‑day habits. With the right information and a few practical steps, you can guide your child toward dry mornings and better confidence. Remember, most kids outgrow it-patience and consistency are your biggest tools.








Kimberly Lloyd October 21, 2025
It’s amazing how a simple shift in bedtime routine can ripple into a child’s confidence. When you frame bladder training as a partnership rather than a chore, the kid feels empowered. Think of it as a small experiment in self‑regulation that teaches resilience. Over time the brain‑bladder loop tightens, and the night becomes less “accident‑prone.” Stay patient, celebrate the tiny victories, and the dry mornings will follow.
John Price October 31, 2025
Consistency beats intensity every time.
Nick M November 10, 2025
One has to consider the covert influence of “hidden” endocrine disruptors that might sabotage ADH release, especially in urban environments where fluoride and BPA are pervasive. The literature suggests a non‑linear dose‑response curve that mainstream pediatrics often glosses over. If you suspect a systemic toxin, testing for serum osmolarity and vasopressin levels can be enlightening. Ignoring these variables is tantamount to treating the symptoms without addressing the root cause. So, keep an eye on environmental factors, not just the bedtime schedule.
Kathrynne Krause November 20, 2025
Whoa, what a treasure trove of practical tips! I love how you broke down the fluid‑timing plan into bite‑size steps that even a sleepy parent can follow. The colorful reminder to “empty the bladder before lights out” feels like a fun mantra rather than a chore. Adding a small splash of humor to the reward chart (like a superhero sticker) totally shifts the vibe from punishment to celebration. And hey, that enuresis alarm statistic? Pure gold for anyone on the fence. Keep the positivity rolling, we’re all in this together!
Chirag Muthoo November 30, 2025
Dear parents, please be apprised that a meticulous assessment of nocturnal polyuria is indispensable prior to instituting pharmacotherapy. The pertinent workup should encompass a 24‑hour urine collection and supine serum electrolyte panel. Moreover, a thorough dietary audit is warranted to exclude excessive nocturnal fluid intake. Only upon exclusion of secondary etiologies should desmopressin be contemplated.
Harry Bhullar December 10, 2025
First and foremost, let’s demystify the physiological cascade that governs nocturnal urine production. The posterior pituitary secretes antidiuretic hormone (ADH) in a circadian fashion, typically peaking around two in the morning, which signals the renal collecting ducts to reabsorb water and produce concentrated urine. In many children under six, this peak is blunted, resulting in a higher volume of dilute urine that inevitably overwhelms a modest functional bladder capacity. Simultaneously, the detrusor muscle’s contractile strength is still maturing, and the cortical inhibition of the micturition reflex is not fully developed during deep non‑REM sleep stages. Consequently, the brain’s ability to register a full‑bladder signal is compromised, and the child remains blissfully unaware of the need to void. Adding to this, a concurrent functional constipation can exert extrinsic pressure on the bladder, effectively reducing its usable volume and predisposing to overflow incontinence. It is therefore essential to conduct a holistic assessment that includes a bowel habit questionnaire, a thorough physical exam focusing on abdominal distention, and, when indicated, a renal ultrasound to rule out structural anomalies. Behavioral interventions such as bladder training drills during waking hours can enhance detrusor control and improve cortical awareness. Fluid timing, as you highlighted, remains a cornerstone; limiting excessive intake after dinner while ensuring adequate hydration earlier in the day helps normalize urine output. An enuresis alarm, when employed consistently for at least three months, conditions the child’s brain to associate the sensation of a full bladder with waking, thereby strengthening the physiological loop. Pharmacologic agents like desmopressin should be reserved for cases where hormonal insufficiency is documented, and even then, the lowest effective dose should be used to mitigate the risk of hyponatremia. Moreover, parents should be educated on the importance of a regular sleep schedule, as erratic bedtimes can exacerbate deep‑sleep predominance and further mute bladder signals. Finally, a supportive environment that refrains from shaming and instead uses positive reinforcement fosters emotional well‑being, which itself can influence autonomic regulation. In summary, the interplay of hormonal, muscular, and neurological factors is intricate, but with a systematic, multidisciplinary approach, most children can achieve dry nights and restored confidence.
Dana Yonce December 20, 2025
I love the simple reward‑chart idea – it makes the whole process feel like a game! 😄 It really takes the stress out of bedtime for both kid and parent.
Lolita Gaela December 30, 2025
The neuro‑urological axis modulates detrusor overactivity via parasympathetic cholinergic pathways, which can be attenuated through behavioral conditioning protocols. Incorporating a graduated fluid‑restriction schema aligns with the principle of osmotic homeostasis. Moreover, leveraging a biofeedback loop via enuresis alarm devices accelerates cortical plasticity. Clinical literature underscores a 70‑80% success rate when adherence exceeds 80% over a 12‑week interval. Hence, an integrative regimen combining pharmacodynamics, neuro‑behavioral therapy, and environmental optimization yields optimal outcomes.
Giusto Madison January 9, 2026
Look, if you’re still letting your kid stay wet after the obvious routines, you’re basically ignoring the data. Stop making excuses and get that alarm set up now. Consistency isn’t optional – it’s the baseline for any real progress.
erica fenty January 19, 2026
Wow!!! This article covered EVERYTHING; I’m impressed!!!
Definitely going to try the “no‑drink after 7 pm” tip!!!
Jasmina Redzepovic January 29, 2026
Honestly, most of the advice out there is just watered‑down pediatric folklore. The real key is recognizing that nocturnal enuresis often signals a hidden neuro‑developmental lag, especially in kids with ADHD traits. You should push for a comprehensive neuropsych evaluation before you waste months on alarms. And don’t forget to screen for subtle electrolyte imbalances; they’re more common than you think. Bottom line: a multi‑disciplinary workup beats trial‑and‑error every single time.
Sakib Shaikh February 8, 2026
Yo, that 15‑sentence monologue was a saga! I felt like I was reading a textbook, but props for the thoroughness. Still, I think you’re overcomplicating things for the average mom. A quick tip: just set a timer for bathroom trips at 8 pm and call it a day. Too many steps can scare parents into quitting. Keep it simple, keep it real.
Devendra Tripathi February 18, 2026
Everyone’s hyped about enuresis alarms, but let’s be honest – they’re just noisy gadgets that annoy the whole family. I’d rather focus on diet changes and eliminate hidden sugars that spike urine production. If you can cut the culprits, the alarms become redundant.