When you start an antidepressant, you’re hoping for relief - not a medical emergency. But if you take too much, or mix it with another medication, your body can flood with serotonin. That’s not just a side effect. It’s serotonin syndrome, a life-threatening reaction that can turn mild jitteriness into seizures, high fever, or death in hours. And most people don’t see it coming.
What Exactly Is Serotonin Syndrome?
Serotonin syndrome happens when your brain and nervous system get too much serotonin. It’s not an allergy. It’s not an overdose in the traditional sense - though that can trigger it. It’s a chemical storm. The body can’t process the excess, and your nerves go into overdrive.
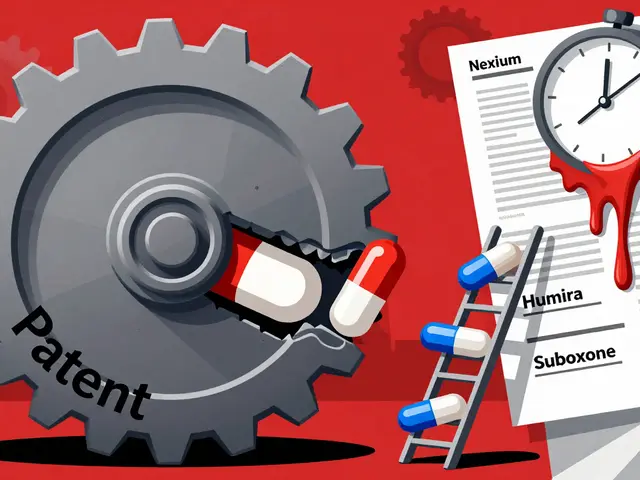
This isn’t rare. Between 2015 and 2022, reported cases rose by 38%, mostly because more people are on antidepressants, and more are taking multiple drugs at once. SSRIs like sertraline or escitalopram cause about 62% of cases. SNRIs like venlafaxine add another 24%. Even tramadol for pain or dextromethorphan in cough syrup can push you over the edge if combined with your antidepressant.
The scary part? Symptoms can hit within an hour. Sixty percent of people feel something wrong within six hours of a new dose or drug interaction. And if you don’t recognize the signs, you might think it’s just anxiety, the flu, or a bad reaction to caffeine.
The Three Clusters of Warning Signs
Doctors don’t diagnose serotonin syndrome by one symptom. They look for patterns - three clear groups of signs that show up together.
1. Mental Status Changes
Confusion, agitation, restlessness, or even hallucinations can be early red flags. You might feel unusually wired, unable to sit still, or suddenly terrified for no reason. In 78% of confirmed cases, people report confusion. In 65%, they’re anxious or agitated - not just sad or low.
If you’re on an antidepressant and suddenly feel like your mind is racing, or you can’t focus even though you’re not stressed, that’s not normal. It’s your nervous system screaming for help.
2. Autonomic Hyperactivity
This is your body’s automatic systems going haywire:
- Heart rate over 100 beats per minute (tachycardia)
- Blood pressure spikes above 160 mmHg systolic
- Body temperature above 38°C (100.4°F)
- Profuse sweating - even if the room is cool
- Dilated pupils (5-8mm, not the normal 2-4mm)
- Rapid breathing (more than 20 breaths per minute)
- Nausea, vomiting, or diarrhea - present in over 60% of cases
These aren’t just uncomfortable. They’re signs your body is overheating and struggling to keep up. If you’re sweating buckets and your heart is pounding, even if you’re lying down, this isn’t stress. It’s a medical alert.
3. Neuromuscular Abnormalities
This is where serotonin syndrome becomes unmistakable - if you know what to look for.
- Clonus: Involuntary, rhythmic muscle contractions. The most telling sign. Try this: gently flex your foot upward. If your toes keep jerking up and down like a metronome, that’s clonus. It’s present in 92% of confirmed cases.
- Tremors: Not just a slight shake. Think hand tremors so strong you can’t hold a cup.
- Hyperreflexia: Your knee-jerk reflex is way too strong. A doctor taps your knee and your leg flies up violently.
- Muscle rigidity: Your limbs feel stiff, locked, like you’re made of wood. This gets worse as the syndrome progresses.
These signs don’t happen alone. The Hunter Criteria - the gold standard for diagnosis - says you need at least one of these combinations:
- Spontaneous clonus
- Inducible clonus + agitation or sweating
- Ocular clonus (eyes darting uncontrollably) + agitation or sweating
- Tremor + hyperreflexia
- Muscle rigidity + fever above 38°C + ocular or inducible clonus
If you see even one of these combos, don’t wait. Call 911.
What Happens If It Gets Worse?
Most cases are mild and resolve within 24-72 hours with treatment. But 30% of patients end up in the hospital. And in the worst cases - about 1 in 20 - things turn critical.
Severe serotonin syndrome can cause:
- Temperature above 41.1°C (106°F)
- Seizures
- Irregular heartbeat or cardiac arrest
- Unconsciousness
- Multi-organ failure
Death happens when your muscles break down (rhabdomyolysis) and your kidneys shut down, or when your brain overheats. The mortality rate? Between 0.5% and 12%. It’s low if caught early. It’s high if you wait.
Real stories from patients on Reddit tell the same tale: they felt off, went to urgent care, and were told they had anxiety. Two hours later, they were in the ER with a fever of 104°F and clonus. They survived - but barely.
What It’s Not: Avoiding the Mistake
Doctors miss serotonin syndrome in 25% of cases because it looks like other things.
Neuroleptic Malignant Syndrome (NMS) - caused by antipsychotics - also causes fever and rigidity. But NMS develops over days, not hours. It causes slow, stiff muscles, not twitching or clonus. Reflexes are weak, not overactive.
Anticholinergic toxicity - from old antidepressants, allergy meds, or sleeping pills - causes dry mouth, no sweating, constipation, and urinary retention. Serotonin syndrome does the opposite: you sweat, you have diarrhea, your pupils are wide.
Don’t assume it’s just “a bad day.” If you’re on an antidepressant and suddenly feel physically wrong - especially with tremors, sweating, or confusion - assume it’s serotonin syndrome until proven otherwise.
What to Do Immediately
If you suspect serotonin syndrome, stop taking all serotonergic drugs right away. That includes:
- SSRIs (fluoxetine, citalopram, etc.)
- SNRIs (duloxetine, venlafaxine)
- MAOIs (phenelzine, tranylcypromine)
- Tramadol, fentanyl
- Triptans (for migraines)
- Dextromethorphan (in cough syrups)
- St. John’s Wort, MDMA, LSD, certain supplements
Then get help. Call 911 or go to the ER. Don’t drive yourself.
In the hospital, treatment is straightforward:
- Stop the drug - immediately
- Give benzodiazepines (like lorazepam) to calm seizures and muscle spasms
- Cool you down with IV fluids and cooling blankets
- Give cyproheptadine - the only antidote - 12mg first, then 2mg every 2 hours until symptoms fade
Most people improve within 24-48 hours if treated fast. Delayed treatment? That’s when organs fail.

How to Prevent It
You don’t have to live in fear. Prevention is simple - but requires awareness.
- Never mix antidepressants without a doctor’s approval. Even “safe” combos like SSRIs and tramadol can trigger this.
- Wait 14 days after stopping an MAOI before starting any SSRI or SNRI. The FDA requires this. Many patients don’t know.
- Tell every doctor - even dentists - what you’re taking. Over-the-counter meds can be dangerous.
- Check labels. Dextromethorphan is in 200+ cough and cold products. Read the “active ingredients” line.
- Ask your pharmacist if a new prescription interacts with your antidepressant. They’re trained for this.
One study showed patient education reduced serotonin syndrome risk by 47%. That’s not a small number. It’s life-saving.
Final Warning
Serotonin syndrome isn’t something you “get used to.” It doesn’t go away on its own. And it doesn’t care if you’ve been on antidepressants for years. One wrong pill, one new painkiller, one extra dose - and it can start.
If you’re on an antidepressant, know the signs. If you feel tremors, sweating, confusion, or your muscles start jerking - don’t wait. Don’t text a friend. Don’t Google it for an hour. Call emergency services. Your life depends on speed.
Antidepressants save lives. But they can also kill if used carelessly. Knowledge isn’t just power - it’s the difference between walking out of the hospital and not walking out at all.
Can serotonin syndrome happen with just one antidepressant?
Yes. While mixing drugs is the most common cause, taking too much of a single antidepressant - especially if you’re not used to the dose or have liver problems - can trigger serotonin syndrome. Overdoses of SSRIs like fluoxetine or sertraline have caused severe cases even without other medications.
How long does serotonin syndrome last?
Mild cases usually resolve in 24-48 hours after stopping the drug and getting treatment. Severe cases can last up to a week, especially if muscle damage or organ stress occurred. The key is early intervention - the sooner you get help, the faster you recover.
Can I get serotonin syndrome from St. John’s Wort or supplements?
Yes. St. John’s Wort is a natural antidepressant that increases serotonin. Mixing it with prescription SSRIs or SNRIs is a leading cause of serotonin syndrome in people who think “natural” means safe. Other risky supplements include 5-HTP, L-tryptophan, and certain energy boosters.
Is serotonin syndrome the same as a panic attack?
No. Panic attacks cause rapid heartbeat, sweating, and fear - but no clonus, no tremors, no muscle rigidity, no fever. If you’re having a panic attack, your body cools down after the episode. In serotonin syndrome, your temperature keeps rising, your muscles keep twitching, and your mind stays confused. Physical signs matter more than how you feel emotionally.
Why don’t doctors always warn patients about this?
Many don’t. A 2023 study found 68% of patients weren’t told about serotonin syndrome when prescribed antidepressants. Doctors assume patients will read the leaflet - but most don’t. Others think it’s rare. It’s not. With rising polypharmacy, it’s becoming more common. If you’re prescribed an antidepressant, ask: “Can this interact with other meds I take? What are the signs of serotonin syndrome?”
Can serotonin syndrome come back after recovery?
Not from the same episode - but you’re at higher risk if you restart the same drug or a similar one too soon. Most doctors wait at least 2-4 weeks after full recovery before considering restarting any serotonergic medication, and even then, they start with a very low dose. Never restart without medical supervision.
Are children and older adults more at risk?
Yes. Older adults metabolize drugs slower, so serotonin builds up faster. Children may be more sensitive to serotonin effects. Both groups are more likely to be on multiple medications - increasing interaction risk. Always be extra cautious with these populations.






Candice Hartley January 27, 2026
I had no idea dextromethorphan could do this. Just last week I took a cough syrup for my cold and was on sertraline. I felt weirdly jittery but thought it was the sugar crash. 😳
April Williams January 29, 2026
People need to stop treating antidepressants like candy. You don't just pop pills and expect your brain to thank you. This is why we have a mental health crisis - because everyone thinks they're a doctor now. You think you're 'just sensitive' but you're one tramadol away from ICU. Wake up.
astrid cook January 30, 2026
I read this and immediately thought of my aunt. She was on venlafaxine and took some St. John’s Wort because her cousin said it was 'natural'. She ended up in the hospital with clonus and a 104 fever. They didn't even know what was happening. This post saved her life. Thank you.
Andrew Clausen January 31, 2026
The Hunter Criteria are not the gold standard. They are a clinical guideline with limited sensitivity in atypical presentations. The DSM-5 criteria are more comprehensive and should be referenced alongside. Also, cyproheptadine is not FDA-approved for serotonin syndrome - it's off-label. Precision matters.
Marian Gilan February 1, 2026
They don't tell you this because they're paid by Big Pharma. The whole antidepressant industry is built on fear. They pump you full of serotonin boosters then scare you with syndrome stories so you keep coming back. And the 'antidote'? Cyproheptadine? That's just another drug they sell. Think about it.
Paul Taylor February 2, 2026
I've been on citalopram for seven years and never had an issue but I never mixed anything. I always told every doctor I saw including my dentist when I needed antibiotics. I also checked every OTC med label. I didn't need to be scared I just needed to be informed. If you're on an antidepressant you owe it to yourself to know what's in your body. Don't wait for a crisis to learn this. Learn it now. Your future self will thank you.
Murphy Game February 4, 2026
This post is a distraction. The real issue is that the FDA approves drugs without proper long-term interaction studies. They let SSRIs go on the market with zero data on polypharmacy risks. Then they slap a tiny warning on the leaflet and call it good. Meanwhile, people die because the system is broken. This isn't about you being careful. It's about them being negligent.
John O'Brien February 4, 2026
I got clonus after taking tramadol with my SSRI and thought I was having a panic attack. I went to urgent care and they gave me Xanax. Two hours later I was in the ER with a fever of 105. They had to cool me down with ice packs and give me cyproheptadine. I'm alive because my roommate knew what to look for. Don't wait. If you feel off and you're on meds - get checked. No excuses.