Hemodialysis Access: What You Need to Know About Vascular Access for Dialysis
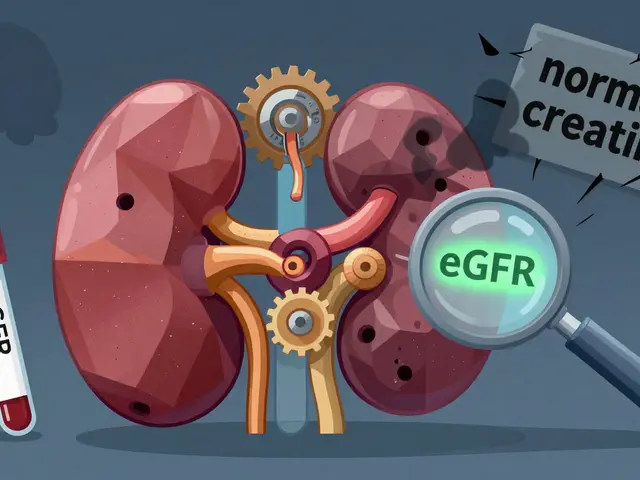
When your kidneys can’t filter blood anymore, hemodialysis access, a surgically created pathway for blood to flow out of and back into your body during dialysis. Also known as vascular access, it’s not just a tube—it’s your connection to life-sustaining treatment. Without it, dialysis can’t happen. And not all access types are created equal.
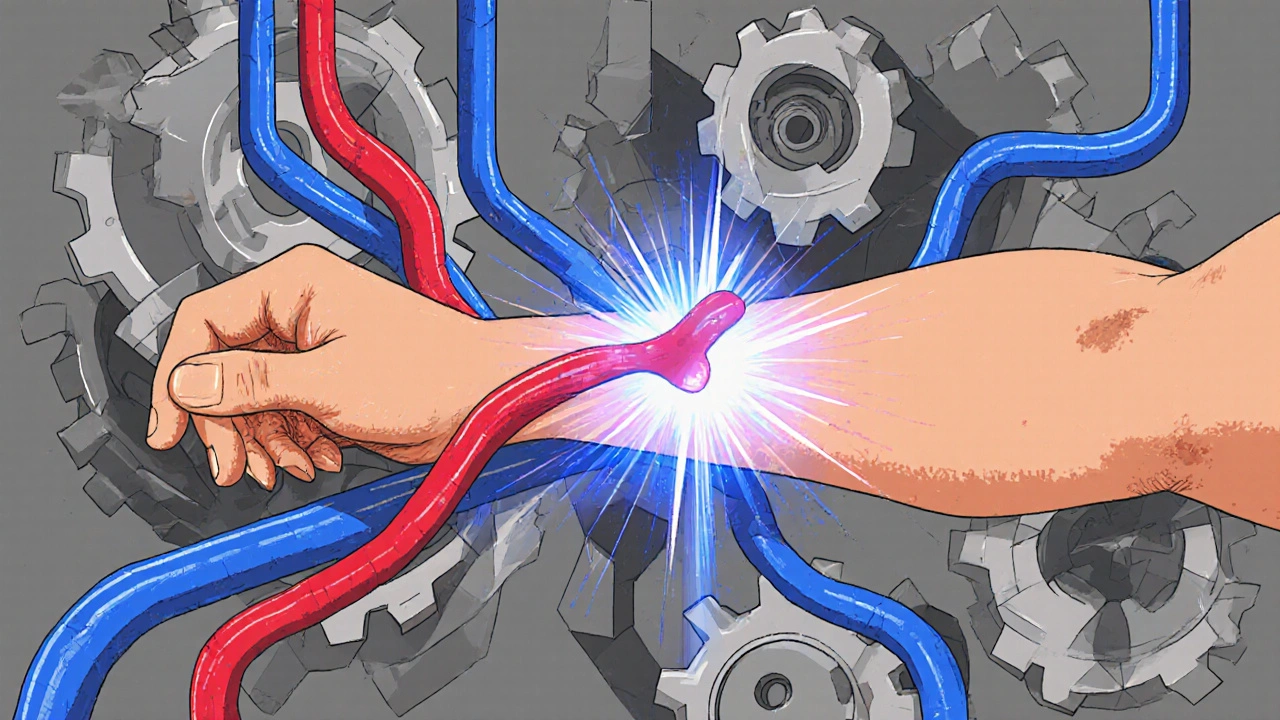
There are three main kinds: fistula, a direct connection between an artery and vein, usually in the arm, which lasts the longest and has the lowest infection risk; graft, a synthetic tube linking artery and vein, used when your veins are too small; and catheter, a temporary or long-term tube placed in the neck, chest, or leg, often used in emergencies but riskier for infections and clots. Most doctors push for a fistula first—it’s the gold standard. But if your veins are damaged from years of IVs or diabetes, a graft might be your only option. Catheters? They’re a stopgap, not a solution.
Getting the right access isn’t just about medical need—it’s about quality of life. A good fistula lets you swim, shower, and sleep without worry. A bad catheter means constant pain, hospital visits, and higher chances of sepsis. People on long-term dialysis often go through multiple access changes. Some need a fistula upgraded to a graft. Others get a catheter removed after their fistula matures. It’s not a one-time fix. It’s an ongoing part of care.
You’ll hear terms like "maturation"—that’s when a fistula grows big and strong enough to handle needles. It can take weeks. Patience matters. No one talks enough about how to protect your access. Avoid tight sleeves, don’t let anyone take your blood pressure on that arm, and check for a buzz or thrill every day. If it’s gone, call your clinic. That buzz means blood is flowing. No buzz? That’s a warning.
The posts below cover real stories and practical advice from people managing dialysis access every day. You’ll find guides on preventing infections, spotting early signs of failure, comparing long-term outcomes, and even how to talk to your doctor when something feels off. Some posts dig into what happens when a graft clots. Others explain why catheters are still used, even with their risks. There’s no fluff—just clear, usable info for patients and caregivers who need to make smart choices, one dialysis session at a time.
Dialysis Access: Fistulas, Grafts, and Catheter Care Explained
Learn the differences between AV fistulas, grafts, and catheters for hemodialysis. Discover which access type is safest, how to care for each one, and why fistulas remain the gold standard for long-term dialysis patients.