Switching to Generics: What You Need to Know Before You Switch
When you switching to generics, the process of replacing brand-name prescription drugs with their chemically identical, lower-cost versions. Also known as generic substitution, it’s one of the most straightforward ways to cut healthcare costs without losing effectiveness. Most people assume generics are just cheaper copies, but they’re not. By law, they must contain the same active ingredient, strength, dosage form, and route of administration as the original. The FDA requires them to work the same way in your body—same absorption, same results. So if your doctor prescribed Lipitor and you switch to generic atorvastatin, you’re getting the exact same medicine, just without the brand name markup.
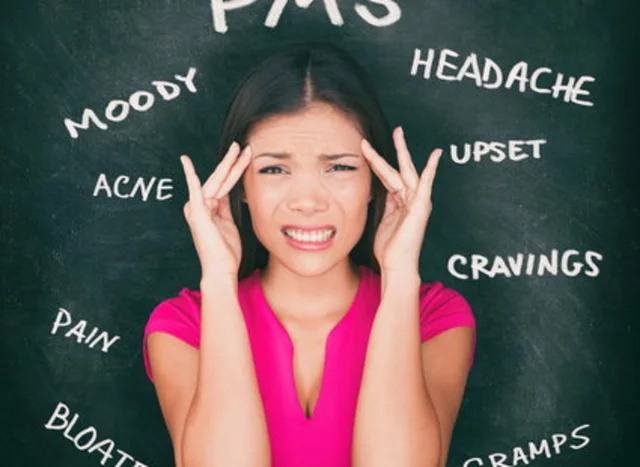
But it’s not always as simple as swapping labels. Some people notice differences when they switch—stomach upset, dizziness, or even a change in how well the drug seems to work. That’s usually not because the generic is weaker. It’s because of inactive ingredients: fillers, dyes, or coatings that vary between manufacturers. These don’t affect the drug’s action, but they can change how fast it dissolves or how your stomach reacts. If you’ve had a bad reaction after switching, talk to your pharmacist. They can check if it’s the filler or if you need to stick with a specific brand’s generic version.
There’s also the question of brand name drugs, originally developed medications protected by patents and sold under proprietary names. Also known as innovator drugs, they’re the reason we pay more for pills that do the same thing as generics. Brands spend millions on marketing and research. Generics skip that. They don’t need to repeat expensive clinical trials—they just prove they’re bioequivalent. That’s why a 30-day supply of brand-name Zoloft might cost $200, while generic sertraline runs under $10 at most pharmacies. The savings add up fast, especially if you’re on multiple meds. And if you’re buying online, the gap widens even more—just make sure the pharmacy is legitimate.
Then there’s generic medications, FDA-approved versions of brand-name drugs that become available after patents expire. Also known as off-patent drugs, they’re the backbone of affordable healthcare around the world. You’ll find them for blood pressure, cholesterol, diabetes, depression, even antibiotics. Many of the posts here cover specific switches—like going from Flonase to generic fluticasone, or from Zoloft to sertraline. People worry about safety, but the data doesn’t support that fear. A 2020 study by the National Academy of Medicine found no significant difference in outcomes between brand and generic drugs across 10 major conditions. The real risk isn’t the medicine—it’s buying from shady online sellers who sell fake generics. Stick to licensed pharmacies. Check for licensing info. Look for real customer reviews. Don’t trust prices that seem too good to be true.
Cost isn’t the only reason to switch. Some insurers push generics hard—sometimes they won’t cover the brand at all unless you’ve tried the generic first. Others offer lower copays for generics. If you’re on a fixed income, or just trying to stretch your budget, switching isn’t just smart—it’s necessary. And if you’re switching because your doctor suggested it, don’t second-guess yourself. They’re not trying to cut corners. They’re trying to keep you healthy without bankrupting you.
Below, you’ll find real-life guides on switching from brand-name drugs to their generic equivalents—from Neurontin to gabapentin, Plavix to clopidogrel, Yasmin to generic birth control pills. Some focus on safety. Others on where to buy cheap, trusted versions. A few warn about red flags you might miss. This isn’t about saving a few dollars. It’s about making sure you get the medicine you need, without paying more than you have to.
Monitoring Your Health After Switching to Generics: What You Need to Watch For
Switching to generic medications is usually safe, but some people notice changes in how they feel. Learn what to monitor, which drugs need extra care, and how to tell if you need to switch back.
When to Call Your Doctor After Switching to Generics: Warning Signs You Can't Ignore
Switching to generic meds saves money, but some people experience side effects or reduced effectiveness. Know the warning signs - like rash, nausea, or worsening symptoms - and when to call your doctor right away.