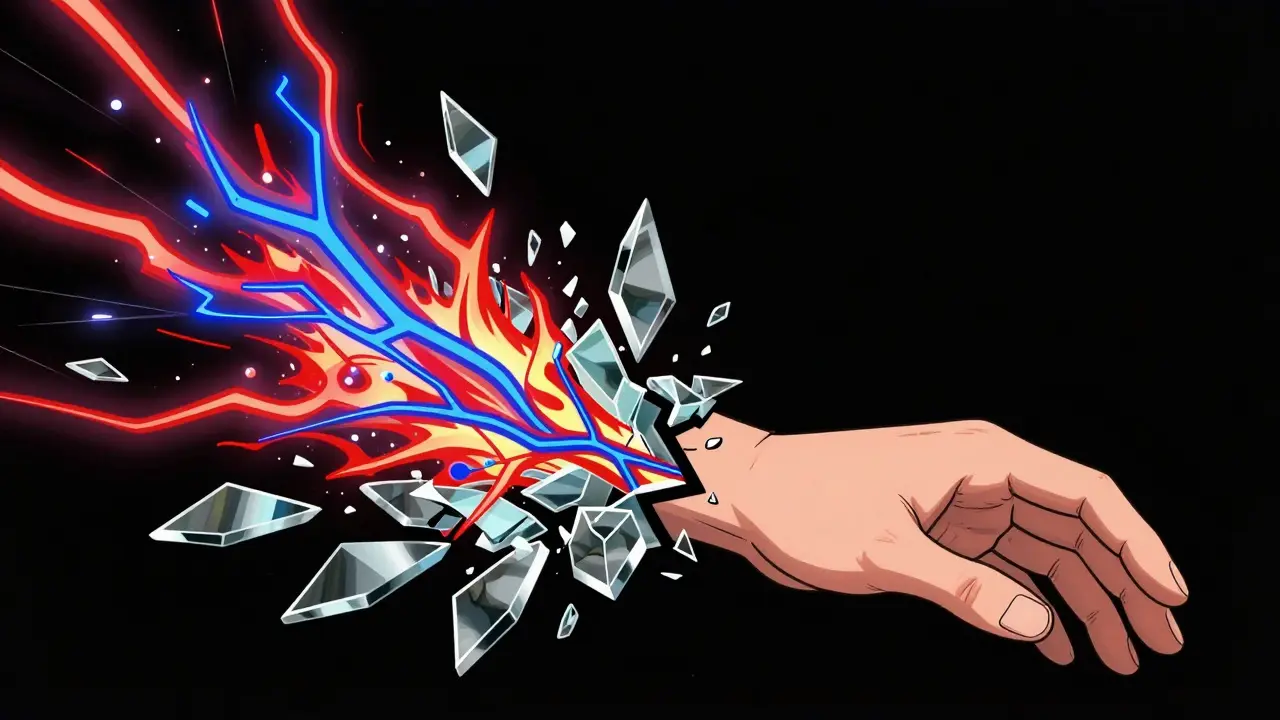
Imagine breaking your wrist. You heal the bone. The cast comes off. But the pain? It doesn’t go away. It gets worse. Your hand feels like it’s on fire-even when you barely touch it. A breeze, a light hug, even the weight of a blanket can feel like a knife. This isn’t normal. This isn’t just healing. This is Complex Regional Pain Syndrome, or CRPS.
It’s Not Just Pain-It’s Your Nervous System Going Rogue
CRPS doesn’t start with a big injury. It often starts with something small: a sprain, a cut, a fracture, even minor surgery. But instead of fading, the pain explodes. It’s not proportional. It’s not logical. It’s your nervous system stuck in overdrive.Most people with CRPS describe the pain as burning, stabbing, or like electric shocks. It’s deep inside the limb-arm, leg, hand, or foot-and it doesn’t match what you’d expect from the original injury. One study found that 40% of CRPS cases follow a fracture, especially wrist fractures. But even people with no clear injury can develop it. The condition isn’t about the wound. It’s about the wiring.
Your nerves, especially the tiny ones that control pain and temperature, get damaged or irritated. Instead of calming down after healing, they keep screaming. Your brain starts listening too hard. The result? Pain signals flood your system, even when there’s no real threat. This isn’t weakness. It’s biology. And it’s real.
What Happens to Your Body Beyond the Pain
CRPS doesn’t just hurt. It changes your body. Early on, your skin might feel warmer or cooler than the other side. It could turn red, purple, or pale. It gets shiny, thin, and sweaty. Your nails grow faster-or stop growing. Hair might grow more or fall out. Muscles twitch. Joints stiffen. You lose fine control. Picking up a spoon becomes impossible.One of the most telling signs? Temperature difference. Studies show the affected limb is often 0.5°C to 1.5°C warmer or cooler than the healthy one. That’s not something you feel in your sleep. It’s measurable. It’s physical. And it’s a red flag doctors look for.
Touch becomes torture. This isn’t just sensitivity-it’s allodynia. A light brush of fabric feels like glass. A change in room temperature triggers a flare-up. You start avoiding anything near the limb. You stop using it. And then, the limb weakens. Muscles shrink. Bones lose density. The more you fear moving it, the more it locks up. It’s a vicious cycle: pain → fear → inactivity → more pain.
Who Gets CRPS-and Why?
CRPS doesn’t pick randomly. Women are three times more likely to develop it than men. It’s most common between ages 40 and 60, but younger people get it too. You don’t have to be old or injured in a car crash. A simple fall, a needle stick, or even a poorly fitted cast can trigger it.Here’s the mystery: why do some people get it and others don’t? Two people break the same bone. One heals fine. The other ends up with burning pain that won’t quit. Scientists think genetics, immune response, and even stress levels play a role. Some research suggests CRPS might involve an autoimmune reaction-your body accidentally attacks its own nerves. A 2022 study found specific autoantibodies in 30% of CRPS patients, pointing to immune system involvement.
One big clue? Timing. CRPS usually shows up 4 to 6 weeks after the injury. If your pain spikes around then, especially if it’s burning and spreading, don’t wait. Early recognition is your best shot at stopping it.
How Doctors Diagnose CRPS-No Scan Can Prove It
There’s no blood test. No X-ray. No MRI that confirms CRPS. Diagnosis is based on symptoms and rules called the Budapest Criteria. These include: pain that’s ongoing and disproportionate, plus at least one symptom from three categories-changes in skin, changes in movement, and changes in temperature or sweating.Doctors also check for asymmetry. Is one hand colder? Is one foot swollen? Is movement restricted? They rule out other things: infections, blood clots, arthritis. If everything else is gone and the pain still screams, CRPS is likely.
Early diagnosis matters. The first 3 months are critical. After that, the nervous system gets harder to retrain. The longer you wait, the more likely the pain becomes permanent.
Treatment: It’s Not One Pill-It’s a Team Effort
There’s no magic cure. But there are tools. And the earlier you use them, the better your chances.Physical therapy is the cornerstone. Not rest. Not avoidance. Movement. Gentle, guided, consistent. You’re retraining your brain to stop seeing the limb as dangerous. A therapist will help you slowly use your hand or foot again-even if it hurts. Pain during therapy doesn’t mean you’re hurting yourself. It means your nerves are learning.
Medications help manage symptoms. NSAIDs like ibuprofen may help early on if there’s inflammation. Corticosteroids can reduce swelling in the first few weeks. For nerve pain, drugs like gabapentin or pregabalin are common. Antidepressants like amitriptyline can calm overactive nerves. Opioids? They rarely help and carry big risks. Most doctors avoid them.
Nerve blocks can interrupt the pain signals. A local anesthetic injected near the spine or affected nerves can give temporary relief and help break the cycle. If that works, some people move to spinal cord stimulation-a device that sends mild electrical pulses to block pain signals before they reach the brain.
Psychological support isn’t optional. Chronic pain rewires your brain. Anxiety, depression, and PTSD are common. Talking to a therapist who understands pain isn’t weakness-it’s part of healing. Cognitive behavioral therapy (CBT) helps you manage fear, reduce catastrophizing, and rebuild confidence in your body.
What Doesn’t Work-and What to Avoid
Too many people are told, “It’s all in your head.” That’s wrong. The pain is real. But some treatments are based on myths.Resting the limb? That makes it worse. Immobilization leads to stiffness, muscle loss, and deeper pain. Don’t wait for the pain to disappear before moving. Move through it-slowly, safely.
Long-term opioids? They don’t fix the nervous system. They just mask it. And they come with addiction risks, tolerance, and side effects. Most pain specialists now avoid them for CRPS.
Alternative therapies like acupuncture or massage? Some people find relief. But they’re not substitutes for evidence-based care. Use them as extras-not the main plan.

Can You Get Better?
Yes. But not always. About half of people with CRPS see major improvement within a year, especially with early treatment. Some recover fully. Others live with milder pain. A smaller group-around 10% to 20%-have pain that lasts for years.Recovery isn’t linear. You’ll have good days and bad days. Flares happen. Stress, cold weather, or even a new injury can trigger them. But with the right team-physiotherapist, pain specialist, psychologist-you can learn to manage it.
The goal isn’t always to be pain-free. It’s to get your life back. To hold your grandchild. To drive. To sleep. To not live in fear of your own body.
What to Do If You Suspect CRPS
If you had an injury, surgery, or trauma-and now you have burning, disproportionate pain that won’t quit:- Don’t wait. See a doctor within 4 to 6 weeks.
- Describe the pain exactly: burning, electric, stabbing, worse with touch.
- Note changes: skin color, temperature, swelling, movement.
- Ask: Could this be CRPS?
- Request a referral to a pain specialist or neurologist.
Bring this information. Print it. Show it. Many doctors still don’t know CRPS well. You might need to educate them.
Hope Is Real-Even When the Pain Isn’t
CRPS is scary. It’s confusing. It’s isolating. But you’re not alone. Thousands live with it. Many have found ways to live well despite it.Research is moving fast. New treatments are being tested-ketamine infusions, immunotherapies, advanced nerve stimulation. The goal isn’t just to treat pain. It’s to stop it before it takes over.
If you’re reading this and you’re in pain, don’t give up. Keep pushing for answers. Find a specialist. Start therapy. Talk to someone who gets it. Your nervous system can heal-even if it feels broken. It just needs the right support.
Is CRPS the same as RSD?
Yes. CRPS used to be called Reflex Sympathetic Dystrophy (RSD). The name changed in the 1990s to reflect a better understanding of the condition. RSD is now an outdated term, but you might still hear it used by older doctors or patients.
Can CRPS spread to other parts of the body?
Yes. In about 70% of cases, CRPS can spread from the original limb to other areas-like from the hand to the shoulder, or from one leg to the other. This is called regional spread. It’s not random; it often follows nerve pathways. Early treatment reduces the chance of spread.
Can CRPS go away on its own?
Sometimes. About half of people see significant improvement without treatment, especially if symptoms are mild and caught early. But waiting is risky. Pain can become chronic, and the nervous system can harden into its overactive state. Treatment greatly improves your odds of full recovery.
Does stress make CRPS worse?
Absolutely. Stress triggers the sympathetic nervous system-which is already overactive in CRPS. Anxiety, sleep loss, emotional trauma, or even arguments can cause flares. Managing stress isn’t optional-it’s part of pain control. Techniques like mindfulness, breathing exercises, and therapy help reduce flare frequency.
Are there any new treatments on the horizon?
Yes. Researchers are testing ketamine infusions to reset pain pathways, immunotherapies targeting autoantibodies, and advanced spinal cord stimulators with smarter programming. Clinical trials are also looking at drugs that block nerve growth factors involved in inflammation. These aren’t available everywhere yet, but they offer real hope for the future.






Anu radha December 18, 2025
This made me cry. I never knew someone else felt this way. My mom had this after a fall, and no one believed her. She just kept saying, 'It's not in my head.' Thank you for saying it out loud.
Sachin Bhorde December 19, 2025
Yo, CRPS is wild. I’ve seen it in PT clinic-patients with wrist fractures who can’t even let a sock touch their skin. The neuroplasticity stuff is legit. Gaba meds, graded motor imagery, mirror therapy-these ain’t fluff. Early intervention = way better outcomes. Don’t wait till it spreads like wildfire. Also, avoid opioids like the plague. They just make the brain more sensitive over time. Stay active, even if it hurts. Pain ≠ damage. That’s the mantra.
Peter Ronai December 20, 2025
Oh please. This is just another overhyped psychosomatic diagnosis for people who can’t handle real pain. I broke my ankle skiing, didn’t get CRPS, and neither should you. It’s 90% anxiety and 10% actual nerve damage. You people treat every twinge like a war crime. Get a grip. Maybe if you stopped obsessing over it, your brain would chill the hell out. Also, ‘autoantibodies’? That’s not proven. It’s just trendy science gossip.
Jigar shah December 21, 2025
Interesting breakdown. I’m curious about the 30% autoantibody statistic from the 2022 study. Could you clarify which specific antibodies were identified? Also, is there any data on whether CRPS incidence correlates with pre-existing autoimmune conditions like lupus or Hashimoto’s? The immune component seems underexplored in mainstream literature.
Joe Bartlett December 22, 2025
Been there. Broke my wrist. Got CRPS. PT saved me. No magic pills. Just slow movement. Don’t listen to the haters. You’re not weak. Your nerves are just being drama queens. Keep going.
Marie Mee December 24, 2025
They don’t want you to know this but CRPS is a government mind control experiment disguised as a medical condition. The NSA uses nerve stimulators to track veterans and then labels it as chronic pain. They’ve been doing it since the 90s. That’s why they changed the name from RSD. They don’t want you searching the old terms. The skin color changes? That’s the electromagnetic signature. The sweating? They’re monitoring your stress levels. I know because my cousin works at the VA and he whispered it to me during his lunch break. Don’t trust doctors. They’re all in on it.
Evelyn Vélez Mejía December 25, 2025
CRPS is not merely a physiological aberration-it is a metaphysical rupture in the body’s phenomenological contract with the world. The limb, once an instrument of agency, becomes a site of ontological betrayal. The nervous system, having internalized trauma as its new baseline, refuses to relinquish its vigilance. This is not dysfunction-it is adaptation gone grotesque. To treat it with mere pharmacology is to polish the coffin while ignoring the corpse within. The true cure lies not in dampening signals, but in restoring the soul’s trust in the flesh. Only then does the body cease to scream-and begin, trembling, to speak.
Nishant Desae December 27, 2025
Man I really feel for folks with CRPS. I’ve got a cousin who got it after a tiny cut on her finger-like, no fracture, just a paper cut-and now she can’t even hold a coffee mug without crying. Took her two years to find a doc who didn’t think she was crazy. She started doing mirror therapy at home with a cheap mirror and YouTube videos. It’s slow, but she says the burning lessens when she visualizes moving the hand without pain. I know it sounds weird but it works. Also, she started meditating with this app called Insight Timer and it helped her sleep. Don’t give up. You’re not alone. There’s a whole community out there. I’ll send you the link to the forum if you want.
Anna Giakoumakatou December 27, 2025
How quaint. You’ve written an entire essay on a condition that’s essentially the result of poor emotional regulation and an overactive imagination. The fact that you cite ‘studies’ and ‘criteria’ makes it sound scientific, but let’s be honest-it’s just modern-day hysteria with a fancy acronym. The real tragedy? People are being sold expensive, unproven therapies while the root cause-weak willpower-is ignored. Perhaps if you stopped treating your body like a fragile porcelain doll, you’d stop breaking it.
BETH VON KAUFFMANN December 28, 2025
CRPS is a catch-all diagnosis for when neurologists run out of differential diagnoses. The Budapest Criteria are vague, subjective, and lack specificity. The so-called ‘temperature asymmetry’? That’s within normal physiological variation. The autoantibody data? Small sample sizes, no replication. And don’t get me started on ‘graded motor imagery’-it’s just exposure therapy with a fancy name. The real issue? Overmedicalization of normal pain persistence. Most patients improve with time and reassurance-not spinal cord stimulators and ketamine.
Raven C December 29, 2025
It is, however, profoundly disheartening to observe the degree to which the medical establishment continues to pathologize subjective experience-particularly in women-under the guise of ‘objective’ criteria. The Budapest Criteria, while ostensibly structured, remain steeped in epistemological bias. The very notion that a patient’s pain must be ‘disproportionate’ to injury implies a hierarchy of suffering, one that privileges the quantifiable over the lived. And yet, we are told to trust this system. How ironic.
Donna Packard December 30, 2025
I’m so glad this exists. I’ve had CRPS for 7 years. Some days are good. Some days I can’t leave the house. But I’m still here. I still hug my kids. I still drive. It’s not perfect, but it’s mine. Keep going. You’re stronger than you think.
Patrick A. Ck. Trip December 31, 2025
Thank you for this. I’ve been researching CRPS since my sister was diagnosed last year. The info here is accurate and compassionate. One thing I’d add: many patients benefit from pacing-breaking activities into tiny chunks, resting before exhaustion hits. It’s not lazy, it’s strategic. Also, cold weather is brutal. Heated gloves, socks, and even heated car seats make a huge difference. Keep advocating. You’re not alone.
Sam Clark December 31, 2025
This is an excellent, clinically grounded summary. I particularly appreciate the emphasis on early intervention and the distinction between pain as a symptom versus pain as a disease state. The integration of psychological support as a core therapeutic pillar-not an adjunct-is critical. For clinicians reading this: refer early. Do not delay. The window for neuroplastic reorganization is narrow, and time is the most valuable, non-renewable resource in CRPS management.
Jessica Salgado January 1, 2026
My daughter got CRPS after a skateboard fall. We were told it was ‘just growing pains.’ Took us 11 months to find a specialist. Now she does PT three times a week. She’s 12. She’s scared. But she’s brave. I wish I’d known this six months ago. Thank you. I’m printing this out and giving it to her school nurse.