Generic Drug Cost Comparison Tool
Compare the cost of brand-name drugs to FDA-approved generics. Most generics cost significantly less while providing identical safety and effectiveness.
When you pick up a prescription, you might see two options: the familiar brand name you’ve seen on TV, or a cheaper generic with a plain label. You might wonder - is the generic just as safe? Is it really the same medicine, or are you risking your health to save a few dollars? The truth is simpler than the fear suggests: generic drugs are not a compromise. They’re the same drug, tested the same way, held to the same standards.
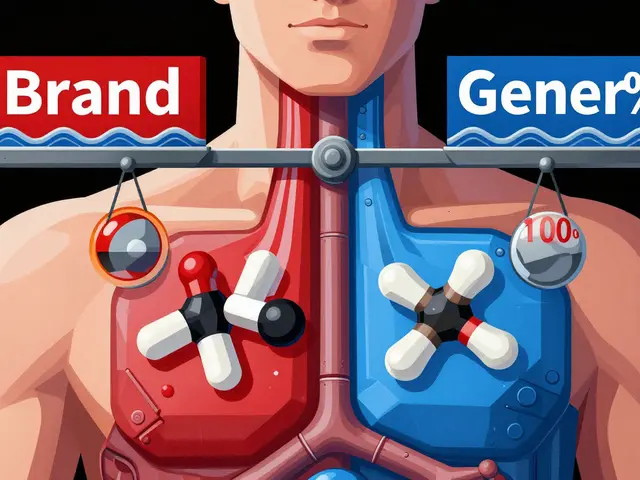
They’re Not Copies - They’re Identical
Generic drugs contain the exact same active ingredient as their brand-name version. If your brand-name pill has 50 mg of lisinopril, so does the generic. Same strength. Same shape. Same way it’s taken - by mouth, injection, patch, whatever. The U.S. Food and Drug Administration (FDA) doesn’t approve a generic unless it proves it delivers the same amount of medicine into your bloodstream at the same rate as the brand. That’s called bioequivalence. The allowed range? Between 80% and 125% of the brand’s absorption. That’s not a wide gap - it’s tighter than the variation you’d see if you took the same brand-name pill on different days.What’s Different? Just the Stuff You Don’t Need
The only differences between a generic and a brand-name drug are the inactive ingredients - the fillers, dyes, and coatings. These don’t affect how the medicine works. They’re there to make the pill hold its shape, taste better, or look different. U.S. trademark laws prevent generics from looking exactly like the brand, so a generic pill might be a different color or shape. But that’s cosmetic. It doesn’t change how it works in your body.Same Factory Standards, Same Inspections
Many people assume generics are made in shoddy factories overseas. That’s a myth. The FDA inspects every facility that makes drugs - brand or generic - and they do it just as often. As of 2023, generic drug plants were inspected every 2.3 years on average. Brand-name plants? Every 2.1 years. The gap is tiny. And the FDA doesn’t care if a factory makes brand or generic - they check for the same things: clean rooms, accurate records, proper testing. In 2022, the FDA approved over 1,000 generic drug applications. Each one had to pass the same quality checks as the original.Cost? A Massive Difference
Here’s where the real story lies: price. A brand-name drug can cost $657 per prescription. The generic? Around $11. That’s not a small saving - it’s life-changing for people on fixed incomes. Generics make up 90% of all prescriptions filled in the U.S., but they only account for 23% of total drug spending. Without generics, millions would skip doses or skip treatment entirely. In 2020, Medicare Part D saved $1.67 trillion just by using generics. That’s not just money - it’s lives kept stable, hospital visits avoided, complications prevented.
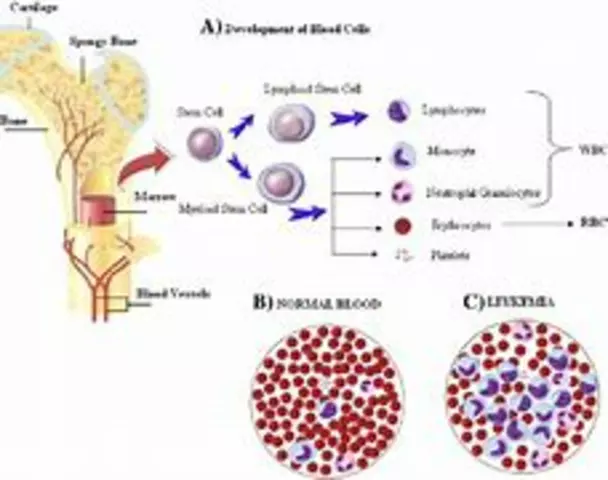
What About the ‘Narrow Therapeutic Index’ Drugs?
There’s one group of drugs where people worry more: those with a narrow therapeutic index (NTI). These are medicines where even a tiny change in blood level can cause problems - too little and the treatment fails, too much and you get toxic side effects. Examples include warfarin (for blood clots), levothyroxine (for thyroid), phenytoin (for seizures), and digoxin (for heart rhythm). For these, doctors and pharmacists are extra careful. The FDA requires additional studies before approving generics for NTI drugs. And yes, some patients report feeling different after switching. But large studies tell a clearer story. A 2019 study of 1.5 million Medicare patients on levothyroxine found no difference in hospital visits, heart problems, or death between those on brand and generic versions. Another study of over 136,000 older adults on blood pressure meds showed a small rise in ER visits after switching - but researchers admitted other factors like age, other meds, or changes in care could explain it. The bottom line? For the vast majority of people, switching to a generic NTI drug is safe. But if you’ve had stable control on a brand-name version and your doctor says, “Stick with it,” listen. That’s not because generics are unsafe - it’s because consistency matters when your body is finely tuned.Why Do Some People Say They Feel Different?
You’ll hear stories. “I switched to generic thyroid meds and I felt tired.” “My blood pressure spiked after the pharmacy changed my pill.” These aren’t made up. But they’re often misinterpreted. First, placebo effect works both ways. If you believe generics are inferior, your brain might make you feel worse - even if the drug hasn’t changed. Second, switching between different generic brands can cause small fluctuations. One generic manufacturer’s version might use a slightly different filler than another. If you’re on a sensitive drug like levothyroxine, switching between two different generics - not just brand to generic - can cause minor hormone shifts. That’s why pharmacists are trained to stick with the same generic brand unless you’re told otherwise. Third, people don’t always realize they’ve switched. Pharmacies often change the generic supplier automatically. You might not notice the pill looks different. You might think the new pill is the problem - when it’s just a different version of the same drug.What Do Experts Really Say?
Dr. Aaron Kesselheim, a professor at Harvard Medical School, put it plainly: “The vast majority of generic drugs are therapeutically equivalent.” The FDA agrees. Janet Woodcock, former head of the FDA’s drug center, said in 2023: “All generic drugs approved by the agency have been shown to work the same way in the body.” Even critics don’t say generics are unsafe. Dr. William Shrank from Humana noted that “subtle differences in inactive ingredients could theoretically affect absorption in certain patients” - but he added that this is rare and mostly relevant for NTI drugs. The real issue isn’t safety - it’s consistency.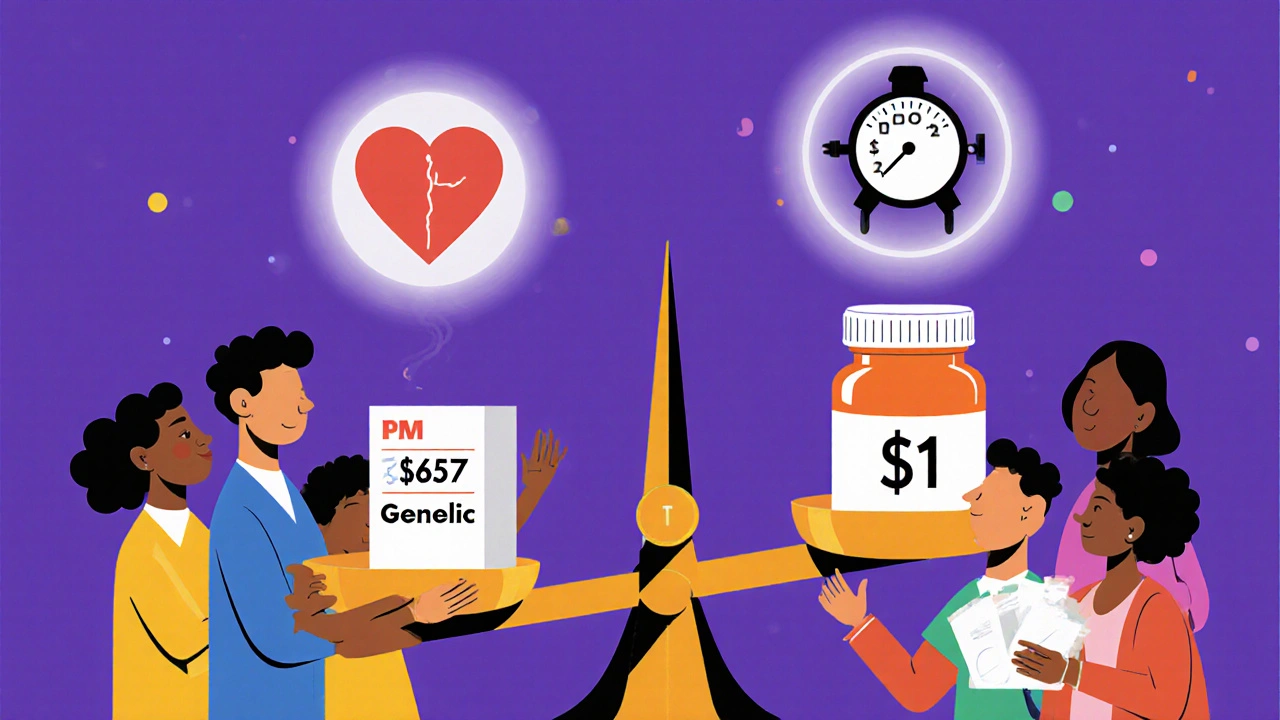
What About the Bad Reports?
You’ll find horror stories online. Reddit threads about thyroid levels going haywire. Drug review sites with low ratings for generics. But numbers don’t lie. The FDA’s adverse event database shows 1.7 reports per 100,000 prescriptions for generics. For brand-name drugs? 1.5. That’s not a difference - it’s noise. And here’s the key: generics are dispensed far more often. So even a tiny increase in reports is magnified by volume. A 2022 Kaiser Family Foundation survey found 68% of Americans believe generics are less effective. Yet 89% of those same people have used them. That disconnect tells you more about fear than facts.What Should You Do?
If your doctor prescribes a brand-name drug, ask: “Is there a generic?” If they say no, ask why. For most drugs, the answer will be yes - and it’s safe. If you’re on a high-risk medication like warfarin or levothyroxine, ask your pharmacist to stick with the same generic brand. Don’t let them switch it without telling you. Keep track of how you feel. If you notice changes - fatigue, dizziness, heart palpitations - tell your doctor. But don’t assume it’s the generic’s fault. It might be something else. If you’re paying out of pocket, choose the generic every time. You’ll save an average of $387 per prescription. That’s not just cash - it’s groceries, gas, rent.What’s Changing Now?
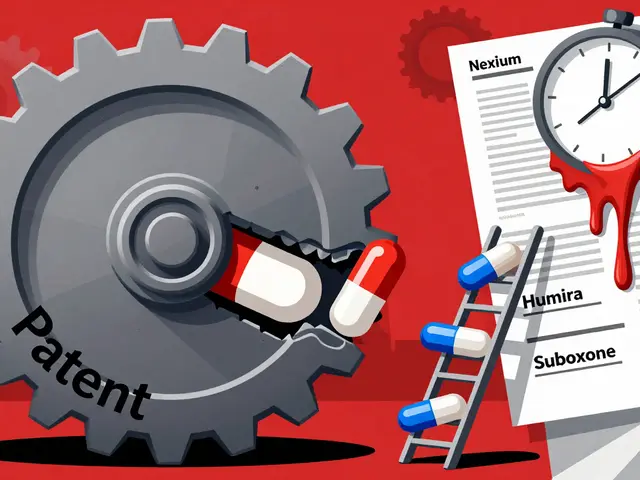
The FDA is stepping up inspections and requiring more data for NTI generics. The 2022 Inflation Reduction Act is pushing for faster generic approvals on Medicare drugs. And more brand-name companies - like Pfizer and Novartis - are now making their own generics. That’s not a conflict of interest - it’s competition. More players mean lower prices and better quality control. Still, there are challenges. In 2022, there were 287 drug shortages - up 17% from the year before. Most were for generic sterile injectables and antibiotics. That’s a supply chain problem, not a safety one. It’s about manufacturing delays, not bad pills.Bottom Line
Generic drugs are not second-rate. They’re not cheaper because they’re worse. They’re cheaper because they don’t need to pay for ads, fancy packaging, or years of research. They’re the same medicine, made to the same rules, tested the same way. For 97% of all generic drugs, the FDA gives them an A rating - meaning they’re fully substitutable. If you’re healthy and taking a common drug - for blood pressure, cholesterol, diabetes, depression - switch to the generic. You’ll save money and get the same result. If you’re on a sensitive drug and feel different after switching, talk to your doctor. But don’t assume the generic is to blame. The science says it’s not. The truth is simple: generics are safe. They’ve saved billions of dollars and countless lives. Trust the data. Not the fear.Are generic drugs as safe as brand-name drugs?
Yes, for the vast majority of drugs. The FDA requires generic drugs to have the same active ingredient, strength, dosage form, and bioequivalence as the brand-name version. They must meet the same manufacturing and quality standards. Over 97% of generic drugs are rated as therapeutically equivalent (A-rated) by the FDA. While minor differences in inactive ingredients exist, they don’t affect safety or effectiveness for most people.
Can switching to a generic drug cause side effects?
For most people, no. Side effects are usually caused by the active ingredient, which is identical in generics. However, a small number of patients on narrow therapeutic index drugs - like levothyroxine or warfarin - may notice subtle changes if they switch between different generic brands. This isn’t because generics are unsafe, but because different fillers can slightly affect absorption. If you feel different after switching, talk to your doctor or pharmacist - don’t stop the medication.
Why do some people say generics don’t work for them?
Often, it’s not the drug - it’s the switch. People may confuse a change in pill color or size with a change in effect. Placebo effects also play a role - if you believe generics are inferior, your body might respond accordingly. Large studies, including one with 1.5 million patients on thyroid medication, show no difference in outcomes between brand and generic. Real-world complaints are usually due to switching between different generic manufacturers, not brand-to-generic changes.
Are generic drugs made in unsafe factories?
No. The FDA inspects all drug manufacturing facilities - brand and generic - with the same standards. In 2023, generic drug plants were inspected every 2.3 years on average. Brand-name plants were inspected every 2.1 years. Many generic drugs are made in the same facilities as brand-name versions. The FDA has issued warning letters to some manufacturers for data issues, but these are rare and apply to both brand and generic producers.
Should I always choose the generic version?
For most medications, yes. Generics save patients an average of $387 per prescription. Unless your doctor specifically says to use the brand - usually because you’re on a narrow therapeutic index drug and need consistency - choose the generic. If you’re paying out of pocket, the savings are significant. Always check with your pharmacist if you’re unsure, and avoid switching between different generic brands unless advised.
What if my insurance won’t cover the brand-name drug?
That’s normal. Most insurance plans require you to try the generic first. If the generic doesn’t work for you - which is rare - your doctor can file an exception request. But for 97% of patients, the generic works just as well. Don’t assume the brand is better. Ask your pharmacist to confirm the generic is FDA-approved and A-rated. You’re not getting a second-rate drug - you’re getting the same one, at a fraction of the cost.









Michelle N Allen November 29, 2025
So I switched my blood pressure med to generic last year and honestly didn't notice a thing
My co-worker swore up and down she felt weird after switching to generic levothyroxine but her doctor said her labs were perfect
Maybe it's just the placebo effect or maybe she was stressed about the switch
I don't get why people act like generics are some kind of scam when the FDA checks them just as hard as the brand names
Craig Hartel November 30, 2025
Love this breakdown. Seriously. I used to be scared of generics too until my grandma started taking them for her diabetes and saved $400 a month
She said she felt the same, slept better, and even started walking more because she wasn't stressed about the cost
Generics aren't just smart economics - they're a lifeline for so many people
Thanks for putting the facts out there without the fear-mongering
Chris Kahanic December 2, 2025
The data presented here is statistically sound and aligns with current FDA guidance documents. Bioequivalence thresholds of 80-125% are well-established and validated through pharmacokinetic modeling. The assertion that generic manufacturing facilities are held to identical standards is corroborated by public inspection reports from the FDA’s Office of Regulatory Affairs. The 2023 inspection frequency differential of 0.2 years is statistically insignificant and reflects random variation in scheduling, not systemic disparity. The conclusion that generics are therapeutically equivalent for the vast majority of indications is empirically supported.
Geethu E December 2, 2025
My mom in India takes generic heart meds and she’s been stable for 7 years
She didn’t even know the difference until I showed her the packaging
Doctors here don’t even mention brand names unless you ask
Why should Americans be scared when the science is the same everywhere?
Stop buying into pharma marketing and start trusting your pharmacist
Bruce Hennen December 3, 2025
You say '97% are A-rated' but you don't mention that the FDA's A-rating system allows for 20% variation in absorption. That's not equivalence. That's a gamble. And don't get me started on the fact that 40% of generic manufacturers have received warning letters in the past decade. You're cherry-picking data to push an agenda.
Chuckie Parker December 4, 2025
Generics are fine if you're okay with being a lab rat for Big Pharma. The FDA is a joke. They approve drugs based on paperwork, not real people. I know someone who had a stroke after switching. Coincidence? Maybe. But I'm not risking my life for $11. You want cheap? Go live in a cardboard box. I'll take my brand name and my peace of mind.
George Hook December 6, 2025
I’ve been on the same generic for hypertension for six years. My doctor switched me from the brand because my insurance wouldn’t cover it. I didn’t feel any different. But I also didn’t switch between different generic manufacturers - I stuck with the same one. That’s the key. The variability isn’t between brand and generic - it’s between different generic suppliers. Pharmacists should be required to notify patients when the manufacturer changes, especially for NTI drugs. Consistency matters more than cost in those cases. And yes, I’ve seen people panic because the pill changed color. That’s not the drug’s fault. That’s a psychological thing. But it’s real to them.
jaya sreeraagam December 7, 2025
Yesss! This is the info we need to spread! I used to think generics were 'cheap junk' until my cousin in Texas got cancer and couldn't afford the brand-name chemo support meds
She switched to generic and kept her treatment on track
She said the only difference was the price tag
And now she’s back to painting and gardening
Don’t let fear steal your health - let common sense save your wallet
Generics are not a compromise. They’re a revolution
Skye Hamilton December 8, 2025
Okay but… what if the generic makes me feel like a zombie? I’m not crazy. I switched and my brain felt like wet cotton. I cried. I called my doctor. I went back to brand. And guess what? I felt human again. So no, I’m not buying your 'it’s all in your head' nonsense. My body knows the difference. And I’m not some lab rat you can just swap out like a lightbulb.
Maria Romina Aguilar December 10, 2025
...I just... I don’t know... I mean, I’ve read all this... and I know the FDA says it’s fine... but... I just... I can’t help it... I feel like I’m being lied to... I’ve been on this one generic for a year... and I keep thinking... what if... what if... I’m just... not... okay...?
Brandon Trevino December 11, 2025
Statistical noise. The adverse event reporting rate for generics is 1.7 per 100,000 versus 1.5 for brands. This is not a clinically meaningful difference. The absolute risk difference is 0.2 events per 100,000 prescriptions - a 13% relative increase, but with a 95% confidence interval spanning from -0.1 to 0.5. The null hypothesis cannot be rejected. Furthermore, the confounding variable of increased volume of generics dispensed (90% of prescriptions) inflates raw counts. The conclusion that generics are not less safe is statistically valid. The emotional anecdotes are irrelevant to population-level safety assessment.
Denise Wiley December 12, 2025
Thank you for writing this. I’ve been so angry about how people treat generics like they’re second-class citizens. My kid has asthma - we switched to generic albuterol and saved $500 a year. He’s still running track. He’s still breathing. The only thing that changed was the price tag. And now I’m telling everyone I know: if your doctor says it’s okay, take the generic. Don’t let fear make you pay more for the same medicine. You deserve to be healthy - and you deserve to keep your money.