When a life-saving drug costs more than a person can afford, who gets to decide if it should be made cheaper? That’s where compulsory licensing comes in. It’s not a loophole. It’s not a secret backdoor. It’s a legal tool written into international law that lets governments step in and allow others to make or sell a patented product - without the patent holder’s permission - when public health is at stake.
What Exactly Is Compulsory Licensing?
Compulsory licensing means the government gives someone else the right to produce a patented invention - like a medicine, vaccine, or medical device - even if the patent owner says no. The patent holder still gets paid. But they don’t get to block access. The key condition: it must serve the public interest.
This isn’t new. The idea dates back to the 1883 Paris Convention, but it was solidified in 1994 by the TRIPS Agreement under the World Trade Organization. Article 31 of TRIPS says countries can issue these licenses under specific rules: pay fair compensation, mostly supply the domestic market, and try to negotiate with the patent holder first - unless there’s an emergency.
And that last part matters. In a pandemic, a national health crisis, or when a drug is simply unaffordable, the requirement to negotiate first can be dropped. Time isn’t a luxury. Lives are on the line.
Why Do Countries Use It?
Mostly for medicines. Between 2000 and 2020, 95% of all compulsory licenses reported to the WTO were for drugs. Cancer treatments. HIV antivirals. Insulin. Vaccines.
Take India. Since 2005, it has issued 22 compulsory licenses for cancer drugs. One of the most famous was for Nexavar, a kidney and liver cancer drug made by Bayer. The price was $5,500 a month. After the license was granted in 2012, a local company started making a generic version for about $175 a month. That’s a 97% drop.
Thailand did something similar in the mid-2000s. They issued licenses for HIV drugs made by Abbott and Bristol-Myers Squibb. Prices fell by 65% to 90%. In Brazil, a compulsory license for efavirenz - an HIV drug - brought the cost per tablet from $1.55 down to $0.48.
These aren’t outliers. They’re examples of how compulsory licensing works when it’s used well: it breaks monopolies, drives prices down, and gets life-saving drugs to people who need them.
How Does It Work in the U.S.?
The U.S. has the legal tools - but rarely uses them.
There are three main paths. First, Title 28, U.S.C. § 1498 lets the federal government use any patented invention - say, a military tech or a vaccine - without permission. The patent owner can sue for compensation in the Court of Federal Claims, but they can’t stop the government from using it. Between 1945 and 2020, only about 10 such licenses were issued - all for government use.
Second, the Bayh-Dole Act of 1980 gives the government “march-in rights” on inventions funded by taxpayer dollars. If a company holds a patent on a drug developed with NIH money and doesn’t make it available or charges too much, the government can step in. Sounds powerful, right? But since 1980, the NIH has received 12 march-in petitions. Not one has been granted. Why? The agency says the company is “taking effective steps” to make the drug available - even if the price is $50,000 a year.
Third, environmental laws like the Clean Air Act allow compulsory licensing if a patented technology is needed to meet pollution standards. But again - rare. The U.S. prefers to rely on voluntary deals, market pressure, or just waiting for patents to expire.

How Do Other Countries Compare?
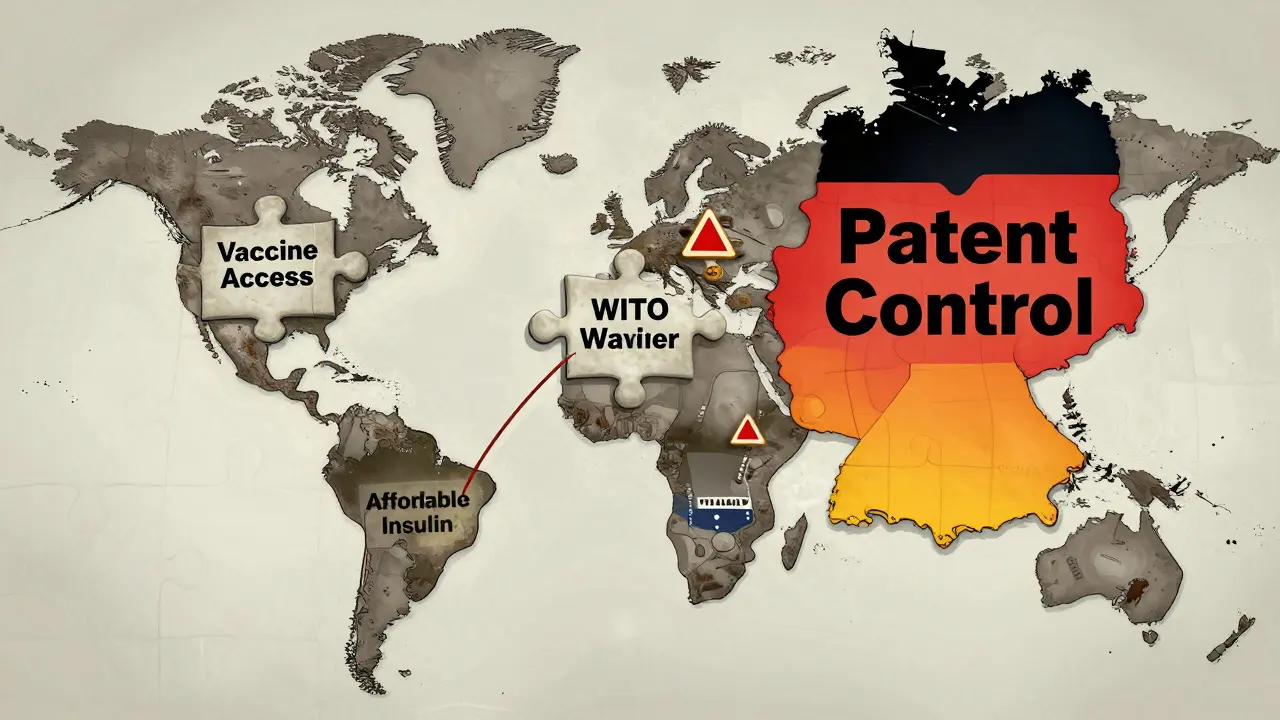
Germany, France, and the UK all have laws allowing compulsory licensing for public health or national defense. But Germany has never issued one. Spain did in 2020, during the pandemic, skipping the negotiation step entirely.
Canada is unique. It’s the only country that’s actually used the WTO’s 2005 export clause - which lets nations with no drug-making capacity import generics made under compulsory license. In 2012, Canada shipped HIV drugs to Rwanda under this rule.
India, Brazil, Thailand, and South Africa have used it more often. Why? Because they’re facing real shortages. They don’t have the same bargaining power as the U.S. or Germany. Their populations can’t wait for voluntary deals to happen.
What Are the Downsides?
Opponents say compulsory licensing kills innovation. The pharmaceutical industry argues that if companies can’t protect their profits, they won’t invest in new drugs. A 2018 study in the Journal of Health Economics found that countries with active compulsory licensing programs saw 15-20% less pharmaceutical R&D investment.
There’s also the legal cost. Bayer fought India’s Nexavar license for eight years. The case went all the way to the Delhi High Court. It’s expensive, time-consuming, and unpredictable.
Then there’s the fear of retaliation. The U.S. Trade Representative puts countries that issue compulsory licenses on its “Priority Watch List.” But since 2012, no country has faced actual trade sanctions over it.
And here’s the real issue: most low- and middle-income countries don’t have the legal teams or technical know-how to even start the process. The WHO says 60% lack the capacity to issue these licenses effectively. So even if the law exists, it’s useless without the expertise to use it.
What’s Changed Since COVID-19?
The pandemic forced a global reckoning. In early 2020, 40 countries - including Canada, Germany, and Israel - prepared or issued compulsory licenses for COVID-related tech. But most never had to use them. Prices dropped anyway, because of public pressure and voluntary deals.
Then came the big one: in June 2022, the WTO agreed to a temporary waiver on vaccine patents. For the next five years, developing countries could make COVID vaccines without permission from Pfizer, Moderna, or AstraZeneca. It was historic. But by October 2023, only 12 facilities in 8 countries had actually started production. Why? Because making a vaccine isn’t just about the patent. It’s about raw materials, equipment, training, and regulatory approval. The patent is just one piece.
Now, the EU is pushing new rules. Their 2023 Pharmaceutical Strategy says if a company doesn’t offer licensing terms within 30 days of a request, the government can skip negotiations and issue a license automatically.
And the WHO is drafting a new Pandemic Treaty. One draft article says: when a public health emergency is declared, essential health products should be automatically licensed. No waiting. No begging. No legal battles.
Who Benefits?
Not the big drug companies. Their stock prices often drop 8% after a compulsory license is announced, according to the IFPMA.
Not the lawyers. Even though it’s a legal process, most applications require specialized patent attorneys - and the average case takes 2.7 years to resolve in the U.S.
Who wins? Patients. Governments. Generic drugmakers. Teva Pharmaceutical made $3.2 billion extra between 2015 and 2020 from markets opened by compulsory licenses.
And the real win? The threat of a compulsory license often forces companies to lower prices voluntarily. Dr. Brook Baker of Northeastern University found that since 2000, the mere possibility of a license led to price cuts on 90% of HIV drugs in poor countries.
Is It the Answer?
Compulsory licensing isn’t a magic bullet. It’s not the first tool you reach for. It’s the last one - when everything else fails.
But when it’s used right, it saves lives. It keeps prices fair. It holds monopolies accountable. And it proves that intellectual property isn’t absolute - it’s conditional. It exists to serve people, not just profits.
The future won’t be about banning compulsory licensing. It’ll be about making it faster, clearer, and more accessible. Especially for the countries that need it most.
Can any country issue a compulsory license?
Yes, any WTO member can - under the TRIPS Agreement. But they must follow specific rules: pay fair compensation, mostly serve their own market, and try to negotiate with the patent holder first - unless it’s an emergency. Some countries, like the U.S., have the law but rarely use it. Others, like India and Brazil, use it regularly for public health.
Does compulsory licensing mean the patent holder gets nothing?
No. The patent holder must be paid “adequate remuneration.” That’s not a fixed amount. It’s based on the economic value of the license. In the U.S., courts use the Georgia-Pacific factors - 15 criteria including royalty rates for similar licenses. In India, the formula is often 6% of net sales. The payment is legally required - it’s not a giveaway.
Why don’t more countries use it if it lowers drug prices?
Three reasons: fear of trade pressure, lack of legal expertise, and the complexity of the process. Even when the law exists, filing a compulsory license requires patent lawyers, health data, government coordination, and often years of legal battles. Many countries simply don’t have the resources. And pharmaceutical companies often threaten lawsuits or delay tactics.
Can compulsory licensing be used for things other than medicines?
Yes. The TRIPS Agreement covers all patents - not just drugs. It’s been used for agricultural chemicals, manufacturing tech, and even assistive devices for the visually impaired under the 2017 Marrakesh Treaty. Canada and India have issued licenses for accessible-format books. But over two-thirds of all cases are still for pharmaceuticals.
Is compulsory licensing the same as piracy or counterfeiting?
No. Counterfeiting is illegal. It’s fake medicine made without authorization, often unsafe. Compulsory licensing is legal. It’s authorized by the government, follows international law, and ensures the product is made to quality standards. The patent holder is paid. The product is regulated. It’s a tool of policy, not crime.
Will compulsory licensing stop companies from developing new drugs?
Studies show a small drop in R&D investment in countries that use it - about 15-20%. But that’s not the whole story. The threat of a license often leads to voluntary price cuts, which still allow companies to make money - just not monopoly profits. And most new drugs are developed in wealthy countries where compulsory licensing is rare. The bigger threat to innovation is not licensing - it’s broken pricing systems that make drugs unaffordable for patients everywhere.