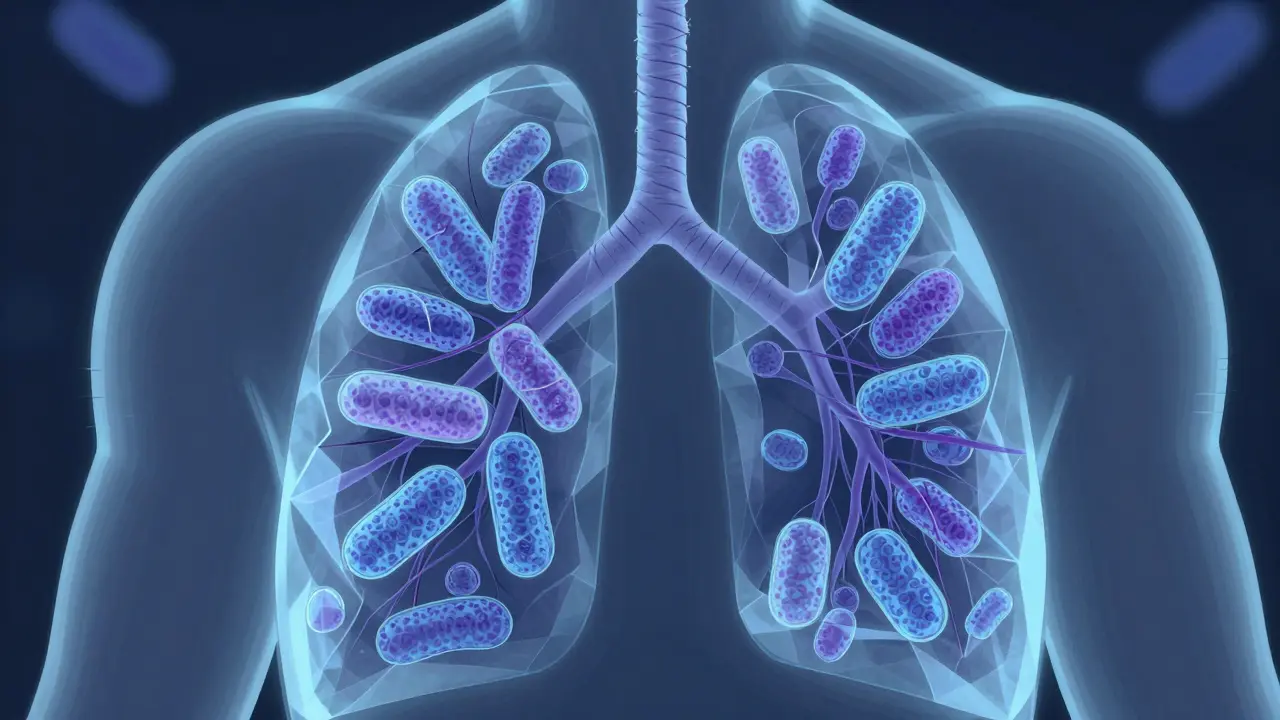
Tuberculosis is a contagious bacterial infection caused by Mycobacterium tuberculosis. It primarily affects the lungs but can spread to other parts of the body. Despite being preventable and curable, TB remains one of the top 10 causes of death worldwide.
Latent TB Infection: The Silent Carrier
Latent Tuberculosis Infection (LTBI) means Mycobacterium tuberculosis bacteria are alive but inactive in your body. You feel fine, show no symptoms, and can't spread TB to others. About 30% of people exposed to TB test positive for infection via tuberculin skin test (TST) or interferon-gamma release assay (IGRA). However, only 5-10% of those with latent TB develop active disease within two years. For people with untreated HIV, this risk jumps to 10% per year. The bacteria hide in granulomas-tiny clusters of immune cells that contain but don’t eliminate the infection.
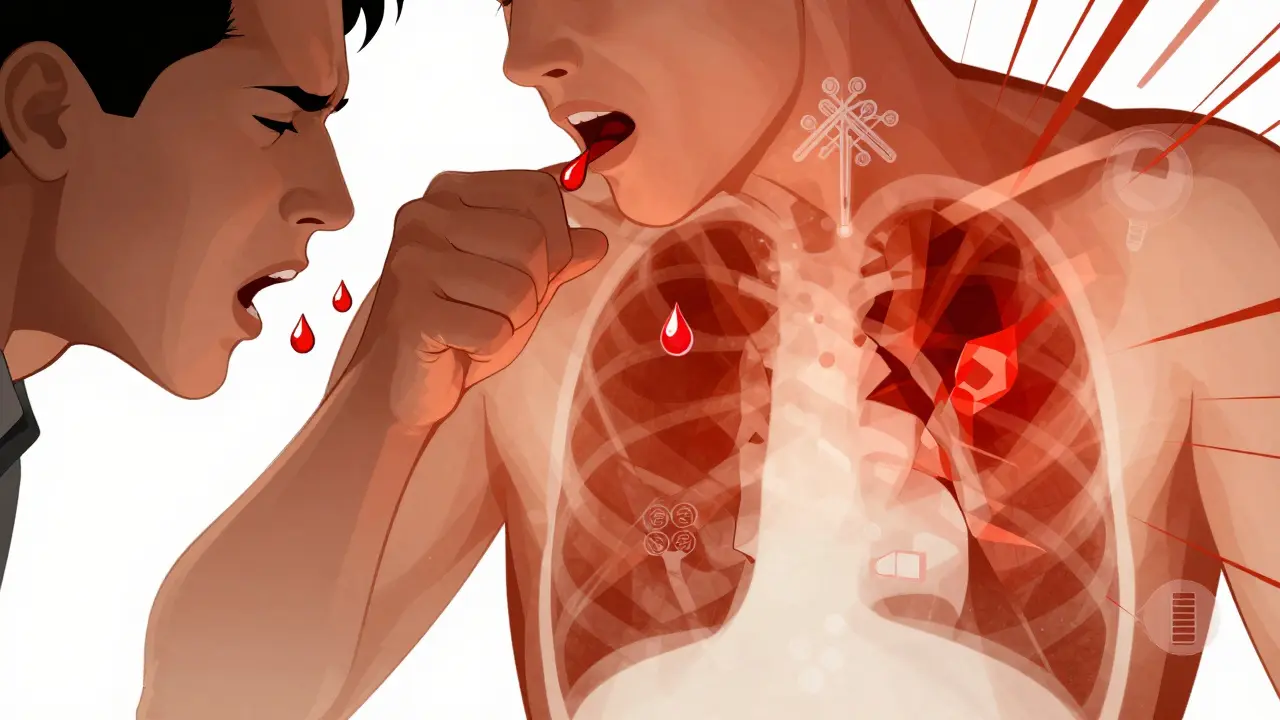
Active TB Disease: Symptoms and Spread
Active Tuberculosis Disease happens when bacteria multiply and damage tissues. Symptoms include a cough lasting over three weeks, unexplained weight loss, night sweats, fever, fatigue, and sometimes coughing up blood. Unlike latent TB, active pulmonary TB spreads through respiratory droplets when coughing or sneezing. Chest X-rays usually show lung abnormalities, and sputum tests confirm bacterial presence. The World Health Organization reports TB caused 1.3 million deaths globally in 2023, with most cases in low-income countries.
Diagnosing TB: How Doctors Tell the Difference
Diagnosis starts with a medical history and symptom check. For Latent TB, doctors use tuberculin skin test (TST) or interferon-gamma release assay (IGRA). A positive result means infection, but no active disease. A normal chest X-ray confirms latency. For Active TB, doctors need positive sputum culture or nucleic acid amplification testing. The CDC emphasizes that active TB requires immediate testing because it’s contagious. Misdiagnosis can lead to severe complications or spread.
Treating Latent TB: Preventing Progression
Latent TB treatment focuses on stopping progression to active disease. Standard therapy is isoniazid for nine months. Newer options include three months of isoniazid and rifapentine (taken weekly) or rifampin for four months. These regimens reduce side effects and improve completion rates. The Minnesota Department of Health notes treatment is critical for high-risk groups like those with HIV or recent TB exposure. Skipping doses risks future active disease.
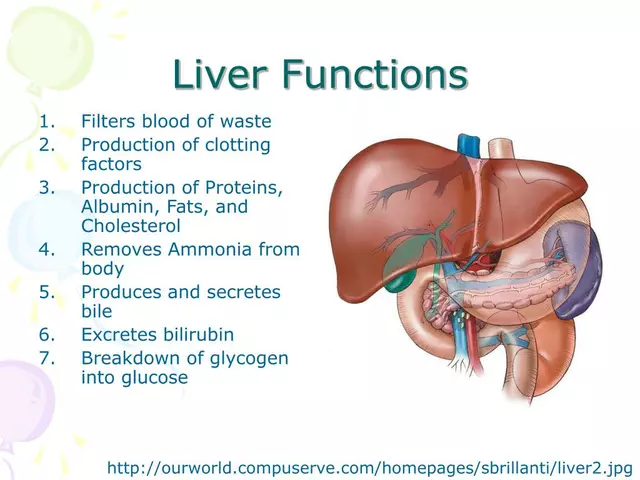
Treating Active TB: The Medication Challenge
Active TB treatment requires a strict four-drug regimen: isoniazid, rifampin, pyrazinamide, and ethambutol for two months. This is followed by isoniazid and rifampin for four to seven months. Directly Observed Therapy (DOT) is recommended-healthcare workers watch patients take every dose. This prevents drug resistance. The CDC states that missing doses can lead to multidrug-resistant TB (MDR-TB), which is harder to treat and costs up to 100 times more than standard therapy. Liver damage from medications requires regular blood tests during treatment.

Why TB Treatment Adherence Matters
Completing TB treatment is non-negotiable. Incomplete treatment causes drug-resistant strains. For latent TB, skipping doses raises the risk of active disease. For active TB, stopping early allows bacteria to survive and mutate. The Georgia Department of Public Health found that patients who completed DOT had 99% cure rates, versus 70% for those who didn’t. Side effects like nausea or rashes are common but manageable. Always talk to your doctor before quitting medication. Public health programs offer support to help patients stay on track.
Current Advances in TB Management
New tools are improving TB control. Nucleic acid amplification tests now diagnose active TB in hours instead of weeks. Shorter latent TB regimens (like three months of isoniazid-rifapentine) boost completion rates. Research into host-directed therapies aims to strengthen the immune system’s fight against TB. The World Health Organization endorsed these innovations to accelerate progress. In the U.S., TB cases hit a historic low of 7,163 in 2020, but disparities persist among foreign-born populations and minority groups. Global efforts now focus on testing high-risk communities for latent TB before it becomes active.
Can you spread TB if you have latent infection?
No. People with latent TB infection cannot spread the disease. The bacteria are inactive and contained within granulomas. Only active pulmonary TB spreads through coughing or sneezing.
Is TB curable?
Yes. Both latent and active TB are curable with proper medication. Latent TB treatment prevents future disease, and active TB requires a full course of antibiotics. Drug-resistant strains need specialized treatment but are still treatable.
Why does TB treatment take so long?
TB bacteria reproduce slowly and hide in hard-to-reach areas like lung cavities. Standard drugs kill active bacteria quickly, but dormant bacteria require prolonged treatment to ensure complete eradication. Stopping early risks relapse or drug resistance.
Can I get TB more than once?
Yes. Even after successful treatment, you can be reinfected with TB. This is why high-risk groups (like those with HIV) need ongoing monitoring. Drug-resistant TB also complicates reinfection risks.
What’s the difference between MDR-TB and XDR-TB?
MDR-TB (multidrug-resistant TB) resists isoniazid and rifampin-the two strongest first-line drugs. XDR-TB (extensively drug-resistant TB) resists those plus at least one second-line injectable drug and a fluoroquinolone. Both require longer, more toxic treatments but are still treatable with specialized regimens.




Laissa Peixoto February 5, 2026
Latent tuberculosis infection is a fascinating paradox of modern medicine.
On one hand, it's a silent carrier state where bacteria lie dormant, contained within granulomas, posing no immediate threat.
On the other hand, this very silence is what makes it so dangerous-because without symptoms, people don't realize they're infected until it's too late.
The fact that 30% of those exposed test positive for latent TB, yet only 5-10% progress to active disease, speaks volumes about the human immune system's resilience.
But for those with compromised immunity, like HIV-positive individuals, that risk skyrockets to 10% annually. It's a stark reminder that health isn't just about individual biology; it's deeply intertwined with social determinants.
Poverty, malnutrition, and lack of access to healthcare all play a role in whether latent TB becomes active.
And yet, despite the availability of effective treatments for latent TB, adherence remains a challenge. Why? Because the medications require months of consistent dosing, and many people stop early when they feel fine.
This is where public health education becomes critical-helping people understand that feeling well doesn't mean the bacteria are gone.
The granulomas aren't a fortress; they're a ticking time bomb. So while latent TB might seem like a minor issue, it's actually a cornerstone of global TB control. Addressing it effectively could prevent countless cases of active disease and reduce the burden on healthcare systems worldwide.
It's a silent battle, but one that we can't afford to ignore. From a philosophical perspective, latent TB forces us to confront the invisible threats in our midst-those that don't show symptoms but still shape our health landscape. It's a lesson in humility for medical science: just because we can't see the problem doesn't mean it's not there.
jan civil February 6, 2026
Latent TB is silent but dangerous. Treatment prevents active disease. Simple.
Dr. Sara Harowitz February 7, 2026
In the United States, we have the most advanced TB protocols! Other countries should follow our lead-especially with DOT and regular testing. Without strict adherence, TB will spread unchecked. It's a national security issue!
Jenna Elliott February 8, 2026
Border controls must be stricter. TB is a foreign threat. We need to quarantine immigrants to protect our citizens. It's not about compassion-it's about survival.
Carol Woulfe February 8, 2026
Ah, yes, the 'simple' solution. But have you considered the pharmaceutical industry's role in prolonging treatment? The real reason TB requires months of medication is to keep people dependent on expensive drugs. The WHO and CDC are complicit in this scheme-why else would they push such lengthy regimens? It's all about profit, not health.
Kieran Griffiths February 10, 2026
TB treatment is tough, but you can do it. Every dose is a step toward victory. Stay strong, and don't hesitate to ask for help. You're not alone in this fight.
Gregory Rodriguez February 10, 2026
Oh, sure, 'stay strong'-because nothing says 'encouragement' like being told to take pills for six months straight. But hey, at least you won't have to worry about being a walking TB factory. Cheers!
Tehya Wilson February 12, 2026
Latent TB is a silent threat. Treatment adherence is critical. Period.