Every year, Americans fill over 3.9 billion prescriptions for generic drugs. That’s nearly nine out of every ten prescriptions written. Yet, these generics make up only 12% of total prescription spending. Meanwhile, brand-name drugs account for just 10% of prescriptions but 88% of the money spent. The math doesn’t lie: generic drugs are saving the U.S. healthcare system hundreds of billions each year.
How Much Are You Really Saving?
In 2024, the average out-of-pocket cost for a generic prescription was $6.95. For a brand-name drug? $28.69. That’s almost five times more. If you take one prescription a month, switching from brand to generic saves you over $260 a year. For someone on three medications? That’s $800 saved annually - money that could go toward rent, groceries, or a dental visit. For uninsured patients, the gap is even wider. Since 2019, the cost of brand-name drugs jumped 50% to an average of $130.18 per prescription. Meanwhile, generic prices dropped 6% to just $6.95. That’s not inflation - that’s a system working as it should. The numbers don’t stop there. Over the past decade, generic and biosimilar drugs have saved U.S. consumers $3.4 trillion. In 2023 alone, they saved the system $445 billion. Think about that: nearly half a trillion dollars in one year, all because patients got the same medicine at a fraction of the price.Why Are Generics So Much Cheaper?
It’s not magic. It’s law. The Hatch-Waxman Act of 1984 created a shortcut for generic manufacturers. Instead of repeating expensive clinical trials, they only need to prove their drug works the same way as the brand-name version. That’s called bioequivalence. No need to retest safety or dosage. Just prove it delivers the same active ingredient, in the same form, at the same strength. That’s why it takes less than half the time and cost to bring a generic to market. Generic companies don’t spend millions on advertising. They don’t pay for patent extensions or lobbying. Their only job is to make the same pill, cheaper. The FDA approved 745 generic drugs in 2024 - the highest number in over a decade. That’s not just progress. It’s competition. And competition drives prices down. In fact, since 2019, total spending on all generic drugs in the U.S. dropped by $6.4 billion - even as more prescriptions were filled. That’s deflation in action.The Brand-Name Price Problem
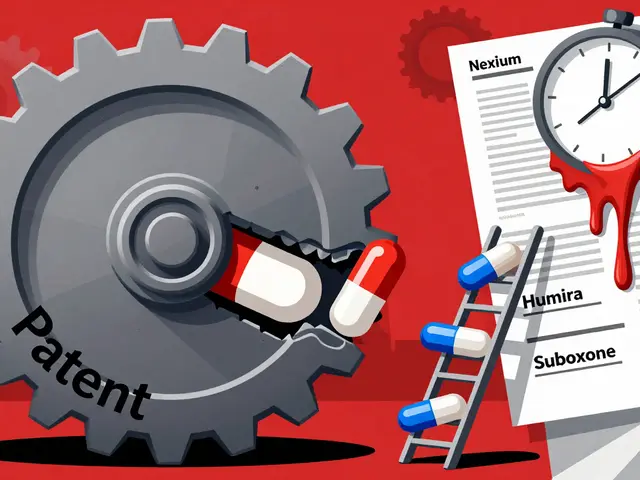
While generics keep getting cheaper, brand-name drugs keep getting more expensive. In January 2025, big pharmaceutical companies raised prices on 250 drugs by an average of 4.5%. That’s nearly double the rate of inflation. Why? Because they can. Many brand-name drugs still hold patents - not just one, but dozens. Some companies file what’s called a “patent thicket.” That’s when they layer on 50, 70, even over 100 patents on a single drug. One heart failure drug, originally set to lose its patent in 2016, kept its monopoly until 2034 thanks to over 75 patents. That’s not innovation. That’s legal obstruction. These tactics delay generic entry. And while generics wait, prices stay high. Blue Cross Blue Shield estimates that “pay-for-delay” deals - where brand companies pay generic makers to stay off the market - cost consumers $3 billion a year. That’s money taken directly from patients’ pockets.
What About Biosimilars?
Biosimilars are the next wave. They’re the generic version of biologic drugs - complex medicines made from living cells, like those used for cancer, arthritis, and Crohn’s disease. Unlike small-molecule generics, biosimilars aren’t exact copies. But they’re proven to work the same way. Since their introduction, biosimilars have saved $56.2 billion in healthcare costs. In 2024 alone, they saved $20.2 billion. One example: Stelara, a treatment for psoriasis and Crohn’s, had a list price of over $5,000 per dose. When nine biosimilar versions hit the market in 2025, prices dropped by up to 90%. Patients who couldn’t afford it before? Now they can. Oncology biosimilars cut cancer drug spending growth in half since 2019. In 2020, they saved $18 billion on cancer care. Yet, even with all this progress, biosimilars still make up less than 30% of the market in competitive areas. There’s room to grow - and more savings to unlock.Why Aren’t More People Using Generics?
You’d think everyone would choose the cheaper option. But barriers remain. First, some doctors still default to brand names. Not because generics don’t work - but because they’re not trained on the latest equivalence data. The FDA’s Orange Book updates monthly with new generic approvals, but many providers don’t check it. Second, pharmacy laws vary by state. Only 42 out of 50 states have modern laws that allow pharmacists to substitute generics without asking the doctor every time. In the other eight, patients might get a brand drug even if a cheaper generic is available - unless they specifically ask. Third, some patients worry. They’ve heard stories about generics not working as well. The truth? Less than 1% of generic prescriptions have any reported issue. The FDA tracks adverse events closely. For drugs with a narrow therapeutic index - like warfarin or levothyroxine - there are stricter rules. But even then, switching between generic brands is safe and common.Who’s Winning? Who’s Losing?
The winners are clear: patients, insurers, Medicare, Medicaid, and employers. A Kaiser Permanente study showed that hospitals using strict generic substitution policies cut pharmacy costs by 25-35% in under two years. Pharmacy benefit managers (PBMs) - the middlemen who manage drug plans - now require generic substitution in 87% of commercial health plans. That’s not just policy. That’s a market signal. The losers? The brand-name drug companies that rely on patent delays and price hikes. Teva, Viatris, and Sandoz - the top three generic makers - control about 35% of the market. But they’re not the enemy. They’re the solution. The real problem isn’t generics. It’s the system that lets brand companies stretch monopolies for decades. The Affordable Prescriptions for Patients Act and the Drug Competition Enhancement Act, both advanced by bipartisan committees in early 2025, aim to end patent thickets and product hopping. If passed, they could unlock another $3 billion in annual savings.
What’s Next?
The patent cliff of 2025 is coming. Three blockbuster drugs - Entresto, Tradjenta, and Opsumit - will lose protection this year. Combined, they brought in $8.6 billion in sales in 2023. Once generics enter, prices will drop by 80-90%. That’s not speculation. It’s history. The FDA expects 12% more first-time generic approvals in 2025 than in 2024. More competition. Lower prices. More access. The Department of Health and Human Services has made bringing biosimilars to patients a top priority. They’re cutting red tape, training doctors, and pushing for transparency. The goal? To make sure the next generation doesn’t have to choose between medicine and rent.What You Can Do
Ask your doctor: “Is there a generic version?” If they say no, ask why. If they say it’s not available, ask if you can get a prescription for the brand and then check prices at different pharmacies. Sometimes, the cash price for a brand drug is cheaper than the copay. Use tools like GoodRx or SingleCare. They show real-time prices for both generic and brand drugs. You might be surprised. If you’re on Medicare, check if your plan has a preferred generic list. Many do - and they offer lower copays. Don’t assume your prescription is locked in. Medications change. Prices change. So should your choices.Are generic drugs really as effective as brand-name drugs?
Yes. By law, the FDA requires generic drugs to have the same active ingredient, strength, dosage form, and route of administration as the brand-name version. They must also prove they’re bioequivalent - meaning they work the same way in the body. Over 90% of prescriptions filled in the U.S. are generics, and adverse event reports show less than 1% of those involve any issue with effectiveness. For the vast majority of patients, generics are just as safe and effective.
Why are generic drugs so much cheaper if they’re the same?
Generic manufacturers don’t have to repeat expensive clinical trials. Thanks to the Hatch-Waxman Act of 1984, they only need to prove their drug is bioequivalent to the brand. They also don’t spend money on advertising, marketing, or patent extensions. With multiple companies making the same drug, competition drives prices down. That’s why a generic can cost $6.95 while the brand costs over $28.
Can I switch from a brand-name drug to a generic without my doctor’s approval?
In most cases, yes - but it depends on your state and your prescription. Pharmacists can substitute a generic for a brand-name drug unless the doctor specifically writes "dispense as written" or "no substitution." Forty-two states have laws allowing this automatic substitution. If you’re unsure, ask your pharmacist. They’re trained to know the rules.
Do generic drugs have different side effects?
The active ingredient is identical, so side effects should be the same. However, generics can have different inactive ingredients - like fillers or dyes - which might cause rare allergic reactions in some people. These are uncommon, and the FDA monitors reports closely. If you notice a change in how you feel after switching, talk to your doctor or pharmacist. But for over 99% of patients, there’s no difference in side effects.
Why aren’t all drugs available as generics?
Some drugs are still under patent protection. Others are complex biologics, which are harder to copy and require biosimilars instead. Patent thickets - where companies file dozens of overlapping patents - also delay generic entry. In 2025, over 150 brand-name drugs are expected to lose patent protection, opening the door for generics. But until then, patients may pay higher prices.









Patrick Jarillon February 7, 2026
Let me tell you something they don’t want you to know - generics are a government scam wrapped in a FDA stamp and sold with a smile. The active ingredient? Sure. But the fillers? The binders? The dyes? Those are different. And guess what? Your body doesn’t care about FDA paperwork. It cares about how it feels. I switched to generic levothyroxine and started having panic attacks. Switched back? Instant relief. They say 99% are fine - but what about the 1% who end up in the ER? You think that’s just bad luck? Nah. It’s systemic neglect. They’re not saving you money - they’re saving Big Pharma from having to innovate. And you’re the guinea pig.
Sarah B February 7, 2026
Generics work fine. Stop overthinking it. I’ve been on them for 12 years. No issues. My blood pressure is stable. My cholesterol is down. My wallet is happy. End of story.
Tola Adedipe February 8, 2026
Man I love how this post breaks it down. The Hatch-Waxman Act was genius. It didn’t just lower prices - it forced innovation into the open. I work in supply chain for a midsize pharmacy chain and we’ve seen generics cut our inventory costs by 40% since 2020. Patients don’t even notice the switch. They just get their meds cheaper. The real villain? Those patent thickets. One company filed 92 patents on a single diabetes drug. Ninety-two. That’s not protection - that’s extortion. We need to dismantle these legal loopholes before they crush another generation.
Heather Burrows February 9, 2026
I’m not saying generics are bad. I’m just saying… maybe there’s a reason brand drugs cost more. Maybe it’s not just advertising. Maybe it’s because they actually *care* about quality control. I mean, think about it - if your life depends on this pill, wouldn’t you want the one with the billion-dollar R&D behind it? Not some factory in India that’s been fined three times for sanitation violations? I’m not anti-generic. I’m pro-safety. And safety isn’t free.
Marcus Jackson February 11, 2026
Bro the FDA doesn’t even test generics anymore. They just look at the brand’s old data and say ‘yep looks good’. That’s not science. That’s a formality. And don’t get me started on biosimilars - they’re basically ‘close enough’ drugs. You think your immune system can’t tell the difference between a real biologic and a knockoff? Wake up. They’re saving money. Not lives.
Lakisha Sarbah February 11, 2026
my pharmacist just switched my med without asking and i had a weird reaction so now i always ask. i dont mind generics but i want to be in the loop. also goodrx saved me $120 last month on my antidepressant. so yeah. do the math. its not hard.
Niel Amstrong Stein February 12, 2026
look. i used to think generics were a compromise. then my dad got cancer. he needed a biologic that cost $18,000 a dose. we couldn’t afford it. then a biosimilar came out. $2,000. same results. same survival rate. he’s alive today because of it. so no. generics aren’t ‘second-rate’. they’re the reason people like my dad don’t have to choose between medicine and rent. stop romanticizing brand-name drugs. they’re not heroes. they’re corporations. and the real heroes? the scientists who made generics possible. and the pharmacists who hand them to you without a second thought.
🫡
Paula Sa February 12, 2026
Just wanted to say thank you for this post. I’ve been working as a nurse for 15 years and I’ve seen patients skip doses because they can’t afford the brand. I’ve seen people cry because they had to pick between insulin and groceries. This isn’t just about numbers - it’s about dignity. The fact that we can save half a trillion dollars a year and still have people suffering? That’s not a healthcare system. That’s a moral failure. Let’s fix the system, not just the prescription.