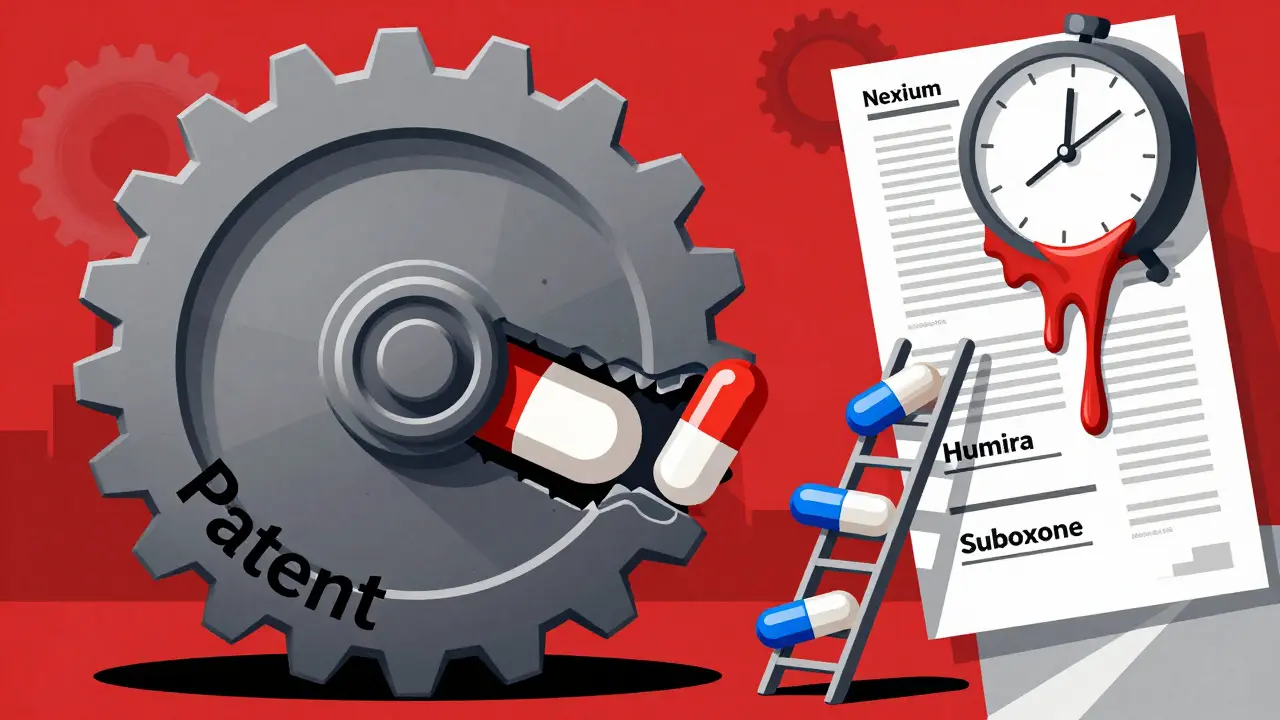
When a blockbuster drug’s patent is about to expire, the company doesn’t just sit back and wait for generics to drop the price by 80%. Instead, they play a long game-filing new patents on tiny changes to the same medicine. This isn’t innovation. It’s evergreening.
What Evergreening Actually Is
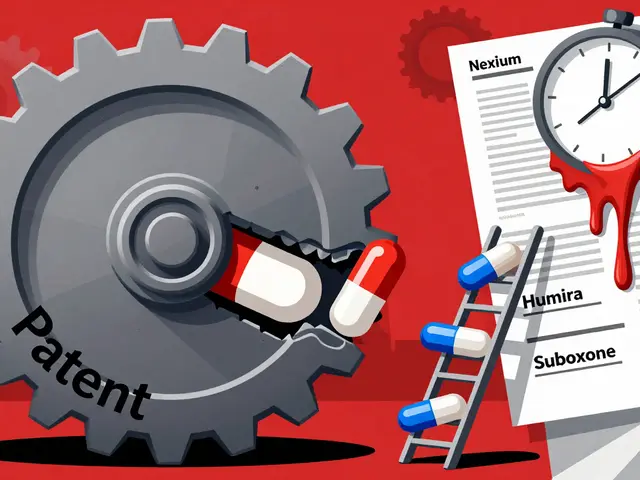
Evergreening is when pharmaceutical companies stretch out their monopoly on a drug by getting new patents on minor tweaks. Think of it like changing the color of your car and calling it a new model. The engine? Same. The performance? Same. But now, you get another 20 years of exclusive sales. This isn’t theoretical. AstraZeneca filed patents on six drugs that added over 90 years of market control. AbbVie’s Humira, a drug for rheumatoid arthritis and other autoimmune diseases, had 247 patent applications tied to it. More than 100 were approved. That’s not innovation-it’s a legal shield. The original patent for a drug lasts 20 years from the date it’s filed. But by the time it hits the market after clinical trials, that clock has already ticked for years. So companies use loopholes to reset the timer. They don’t need to invent a new drug. They just need to tweak the dosage, switch from a pill to a liquid, add a new combination, or change how it’s released in the body.How It Works: The Playbook
Here’s how it plays out in real life:- New formulation: Prilosec (omeprazole) was a daily pill for acid reflux. AstraZeneca switched to Nexium (esomeprazole), which is just one half of the original molecule. It worked the same way-but they patented it as a new drug. Nexium became a $5 billion-a-year product.
- New delivery system: A drug that used to be taken twice a day gets turned into a slow-release version. One pill a day. Sounds better? Maybe. But it’s the same active ingredient.
- Pediatric extension: If a company runs new studies on how a drug affects children, they get six extra months of exclusivity. Sometimes, these studies are done just to buy time.
- Orphan drug status: If a drug is repurposed for a rare disease-even if it’s already on the market for something common-it gets seven years of exclusivity.
- Product hopping: Companies stop making the original version. They push doctors and pharmacies to switch to the new version. Then they sue generics trying to sell the old one.
Why It Matters: The Real Cost
Generic drugs cut prices by 80-85% within a year of launch. That’s not a guess. That’s what happens every time. But evergreening blocks that from happening. Humira costs about $70,000 a year in the U.S. In Canada, where generics came in faster, the same drug costs $5,000. That’s not because of manufacturing differences. It’s because of patents. Patients with autoimmune diseases, diabetes, or heart conditions are stuck paying hundreds or thousands of dollars a month for drugs that could be $50 a month. Some skip doses. Some skip meals. Some just don’t fill the prescription. And it’s not just individuals. Medicare, Medicaid, and private insurers pay the difference. In 2022, the U.S. spent over $1.4 trillion on prescription drugs. A huge chunk of that went to drugs protected by evergreening.
Who’s Doing It-and Who’s Fighting Back
AstraZeneca, AbbVie, Pfizer, and Johnson & Johnson are the biggest players. But it’s not just big names. Almost every major pharma company uses these tactics. The Federal Trade Commission (FTC) sued AbbVie in 2022, calling Humira’s patent strategy an “anticompetitive scheme.” The lawsuit said AbbVie used over 100 patents to block generics for more than a decade. The case is still ongoing. The Inflation Reduction Act of 2022 started letting Medicare negotiate prices for some of the most expensive drugs. That’s a direct threat to evergreening. If the government can cap the price, the financial incentive to delay generics shrinks. In Europe, regulators now require proof of “significant clinical benefit” before granting extra exclusivity. That’s harder to fake than just changing a pill’s coating.Is There Any Legitimate Use?
Some argue that evergreening encourages companies to keep investing. But here’s the truth: developing a new drug costs $2.6 billion and takes 10-15 years. Evergreening costs a fraction of that. A patent attorney and a chemist can file a new patent for under $100,000. The real innovation happens in early-stage research. Evergreening is about protecting revenue, not creating better medicine. There are cases where a small change makes a real difference-like reducing side effects or making a drug safer for elderly patients. But those are rare. Most of the time, the new version is no better than the old one.
What’s Next?
The next wave of evergreening is even sneakier:- Supragenerics: A company creates its own generic version of its drug and sells it under a different brand. That blocks other generics from entering.
- Pharmacogenomics: Patenting a genetic test that says “this drug only works for people with this DNA marker.” Then, only your version gets covered by insurance.
- Biologics and nanotech: These drugs are harder to copy. Companies are filing patents on delivery systems that make generics nearly impossible to replicate.
What Can You Do?
If you’re taking a brand-name drug that’s been on the market for more than 10 years, ask your doctor or pharmacist: Is there a generic version available? If they say no, ask why. Chances are, it’s because of a patent trick. You can also check if your state has a drug affordability program. Some states now track evergreening and push for faster generic access. And if you’re part of a patient advocacy group or health nonprofit, support efforts to reform patent law. The current system isn’t broken-it was built this way.What’s the Alternative?
Instead of letting companies extend monopolies with tiny changes, we could reward real innovation. Give companies a cash prize for developing a truly new drug. Or let them keep higher prices for five years, then open the market. That’s what other countries do. The U.S. is one of the last holdouts. The truth? We’re paying for patents, not progress.Is evergreening legal?
Yes, for now. Evergreening exploits loopholes in patent law, especially under the Hatch-Waxman Act. While courts and regulators are starting to challenge it, most tactics are still technically legal-even if they’re widely criticized as abusive. The system allows patenting of minor modifications as long as they meet the low bar of being "non-obvious," which many experts argue they aren’t.
How does evergreening affect drug prices?
Evergreening keeps prices high by delaying generic competition. Once generics enter the market, prices typically drop by 80-85%. By blocking that entry for years, companies maintain monopoly pricing. For example, Humira cost $70,000 a year in the U.S. while generics in Canada cost under $5,000-same drug, same manufacturer, different patent rules.
What’s the difference between evergreening and real innovation?
Real innovation means discovering a new molecular compound that treats a disease in a new way. Evergreening means tweaking an existing drug-changing the dosage form, adding a second ingredient, or altering release timing. The clinical benefit is often negligible. While innovation costs billions and takes over a decade, evergreening costs under $100,000 and takes months.
Which drugs are most commonly evergreened?
Blockbuster drugs with high sales volume and long market life are prime targets. Examples include AstraZeneca’s Prilosec/Nexium (GERD), AbbVie’s Humira (autoimmune diseases), and Indivior’s Suboxone (opioid addiction). These drugs generate billions annually, so even a few extra years of exclusivity mean billions in extra profit.
Are there any countries that stop evergreening?
Yes. The European Medicines Agency requires proof of "significant clinical benefit" before granting extended exclusivity. India and Brazil also reject patents on minor modifications under their patent laws. Canada and Australia have stricter standards than the U.S. for what counts as a new invention. These countries allow generics to enter faster, lowering drug costs for their populations.
Can patients fight evergreening?
Patients can’t directly stop patent filings, but they can push for change. Ask your doctor if a generic is available. Support advocacy groups that challenge drug pricing. Contact your representatives about patent reform. When enough people demand transparency, regulators and lawmakers respond. The FTC’s lawsuit against AbbVie started because patients and providers spoke up.







kabir das January 30, 2026
Oh my GOD, this is insane!!! I can't believe they're just changing the color of the pill and calling it a NEW DRUG!!! This is like selling the same car with a new paint job and charging $50k more!!!
rajaneesh s rajan January 31, 2026
Yeah, it's not innovation-it's intellectual property theater. They're not curing diseases, they're gaming the system. The real tragedy? People are dying because they can't afford the $70k version of a $50 drug. And we call this capitalism? More like corporate feudalism.
Pawan Kumar February 1, 2026
One must consider the broader macroeconomic implications of patent law erosion. The pharmaceutical industry operates within a framework of intellectual property rights designed to incentivize R&D. To dismantle evergreening without introducing a viable alternative is to risk the collapse of innovation infrastructure. One cannot simply abolish property rights and expect continued medical advancement.
Kacey Yates February 3, 2026
so like... if you change the pill from blue to red and call it nexium and charge 10x more... thats legal?? why is no one in jail??
ryan Sifontes February 4, 2026
theyre all in on it. the fda, the congress, the doctors. its all rigged. you think they care if you live or die? nope. they just want their cut.
Laura Arnal February 5, 2026
This is so heartbreaking 😢 I have a friend with RA who skips doses because she can't afford Humira. We need change. And it's not just about money-it's about dignity. Let's push for reform! 💪❤️
Jasneet Minhas February 6, 2026
One cannot help but observe the absurdity of this system. A molecule, unchanged in its pharmacological essence, is rebranded with a new formulation and marketed as revolutionary. The irony? The very patients who depend on these drugs are the ones who pay the price-for nothing but legal fiction.
Eli In February 8, 2026
It’s wild how the U.S. is the only rich country that lets this happen. In Canada, Germany, Australia-people get affordable meds. Here? You need a second job to afford insulin. We’re not just broken-we’re outliers in cruelty.
Megan Brooks February 9, 2026
While the ethical concerns are undeniable, we must also acknowledge the complexity of patent law and the role of litigation in shaping market access. Reform efforts must be nuanced, balancing innovation incentives with equitable access. A blanket condemnation risks unintended consequences.
Paul Adler February 10, 2026
I’ve seen this firsthand. My dad was on Prilosec for years. Then they switched him to Nexium-same side effects, same results, double the cost. The pharmacist just shrugged and said, ‘That’s what the script says.’ We didn’t know any better. That’s the problem.
Robin Keith February 12, 2026
It's not just about patents-it's about the entire ideological architecture of late-stage capitalism, where human health is commodified, where the body becomes a ledger, where the soul is priced per milligram. Every patent filing is a silent scream of a system that values profit over personhood. And we-every one of us-participate in it by paying, by not protesting, by accepting the narrative that this is just how things are.
Doug Gray February 13, 2026
The structural inefficiencies inherent in the U.S. healthcare ecosystem are exacerbated by regulatory capture. The FTC's litigation against AbbVie is a symptomatic intervention, but without dismantling the patent-thicket paradigm, we're merely rearranging deck chairs on the Titanic.
Kristie Horst February 13, 2026
How is it that we, as a society, have allowed this to become normalized? We celebrate innovation, yet we reward manipulation. We honor science, yet we enable legal fiction. The disconnect between our values and our systems is not accidental-it is engineered.
LOUIS YOUANES February 15, 2026
They’re not even trying to hide it anymore. It’s like watching a magician say ‘I’m gonna pull a rabbit out of my hat’ and then pulling out a rabbit. And everyone claps because they think it’s magic. It’s not. It’s fraud. And we’re paying for the ticket.
Andy Steenberge February 16, 2026
There’s a real opportunity here for patient advocacy groups to partner with state legislators to create transparency dashboards-showing which drugs are being evergreened, how many patents were filed, and how long generics were delayed. Knowledge is power. Let’s make this data public.