When your kidneys aren’t working right, even common medicines can turn dangerous. It’s not about taking too many pills-it’s about your body not being able to clear them. For someone with chronic kidney disease (CKD), a standard dose of ibuprofen, metformin, or even an antibiotic can build up to toxic levels. This isn’t rare. It happens every day in clinics and hospitals, often because no one checks the eGFR.
Why Kidneys Matter for Medicines
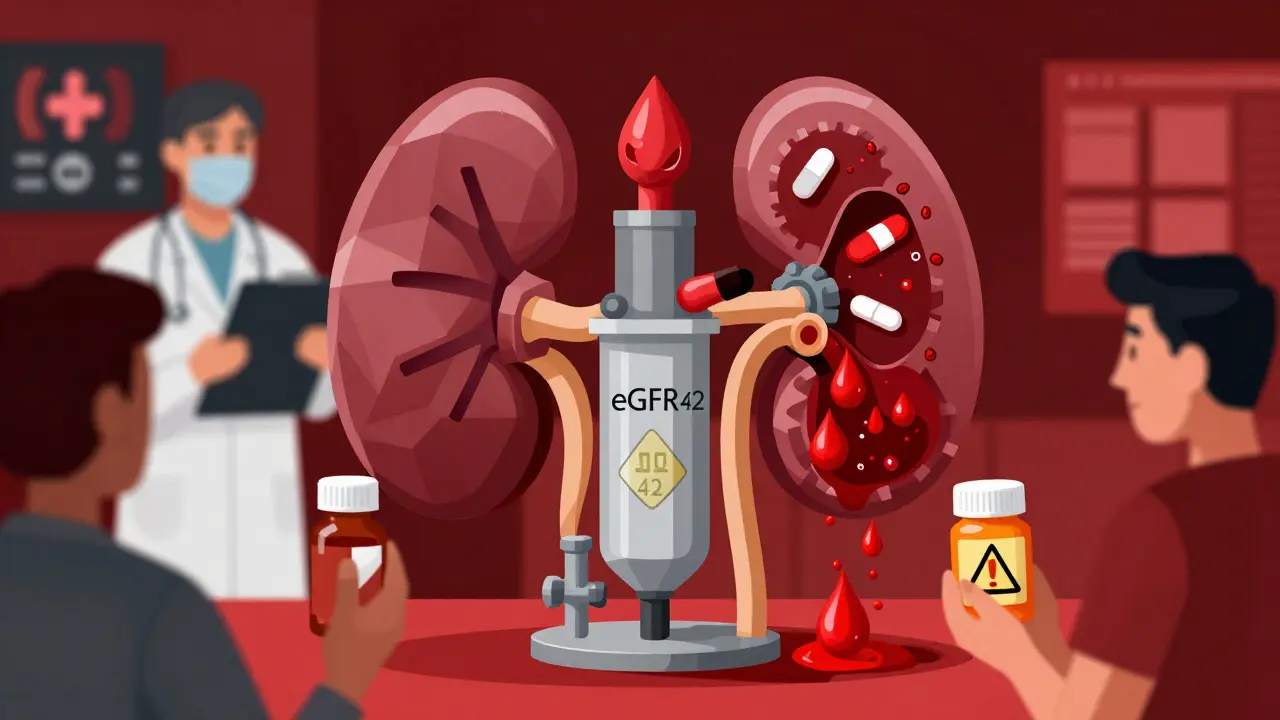
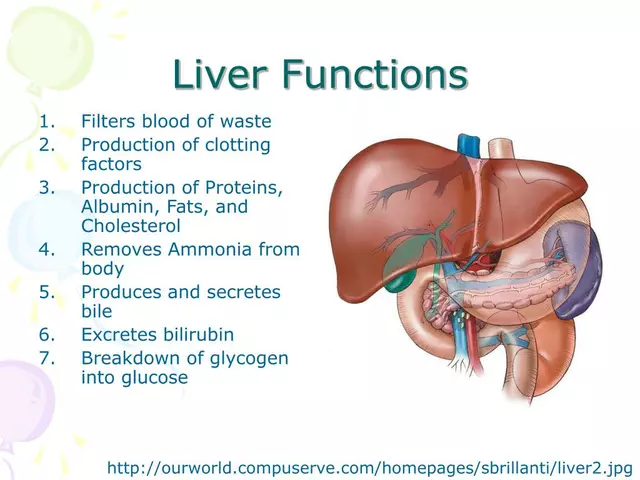
Your kidneys don’t just make urine. They filter about 30% of all prescription and over-the-counter drugs out of your blood. When kidney function drops-say, from an eGFR of 90 to below 60 mL/min/1.73m²-your body can’t flush out meds like it used to. That’s when levels rise, slowly and silently. You might feel dizzy, confused, or just "off." But the real danger? Organ damage, hospital stays, or worse.It’s not just about the kidneys filtering. Some drugs are broken down by the liver but still need healthy kidneys to remove the leftovers. Others, like vancomycin or trimethoprim, are cleared almost entirely by the kidneys. If you have stage 3 CKD (eGFR 30-59), 40% of commonly prescribed drugs need a dose change. By stage 4 (eGFR under 30), that number jumps even higher.
Top 5 Medications That Turn Toxic in Kidney Disease
- NSAIDs (ibuprofen, naproxen, diclofenac): These painkillers cut blood flow to the kidneys. In someone with eGFR under 60, they raise the risk of acute kidney injury by three times. One Reddit user with stage 3 CKD saw their creatinine spike from 1.8 to 3.2 after taking standard ibuprofen for back pain. They ended up hospitalized for five days.
- Metformin: The go-to diabetes drug. But when eGFR drops below 45, it needs a lower dose. Below 30? Stop it. Why? Risk of lactic acidosis-a rare but deadly buildup of acid in the blood. Still, a Cochrane review of 20,000 patients found no cases when guidelines were followed.
- Sulfonylureas (chlorpropamide, glyburide): These diabetes pills cause low blood sugar. In advanced CKD, chlorpropamide’s half-life balloons from 34 hours to over 200 hours. Glyburide’s metabolites hang around for days. Patients wake up confused, sweating, even seizing from hypoglycemia-despite eating normally.
- Trimethoprim (and co-trimoxazole): Used for UTIs and infections. But when combined with ACE inhibitors or ARBs (common in CKD patients), it can spike potassium by 1.2-1.8 mmol/L in under 48 hours. High potassium can stop your heart.
- Aciclovir: An antiviral for shingles or cold sores. In CKD, it forms crystals in the kidney tubules. Up to 15% of patients with eGFR under 50 get crystal nephropathy. Some develop confusion or seizures from drug buildup.
How Doctors Miss the Warning Signs
Many providers still check serum creatinine alone. That’s like checking the oil light without looking at the gauge. Creatinine can look normal even when kidney function is half gone-especially in older adults, women, or people with low muscle mass.A 2022 JAMA Internal Medicine study found 35% of primary care visits didn’t calculate eGFR. That’s a massive gap. Even worse? Forty-two percent of pharmacists and prescribers fail to adjust doses for drugs cleared more than 50% by the kidneys when eGFR is under 60. That’s not negligence-it’s a system failure.
Drug labels say "use with caution in renal impairment." But what does that mean? No numbers. No guidance. That’s why tools like the UCSF Renal PharmPK database and the University of Florida’s Renal Dosage Handbook exist. They give exact dose adjustments for 512 medications across five CKD stages.
What Happens When You Don’t Adjust Doses
The American Society of Nephrology says drug-induced acute kidney injury (AKI) happens in 19-29% of hospitalized patients. Mortality? 1.8 times higher than non-drug-related AKI. And 38% of these cases are preventable.Take vancomycin. Standard dose: 15 mg/kg every 12 hours. In stage 5 CKD? Every 48-72 hours. Trough levels must be monitored at 15-20 mcg/mL-not the usual 10-15. Miss that, and you risk hearing loss, kidney damage, or both.
Or contrast dye for CT scans. In CKD patients, it causes contrast-induced AKI in 12-18% of cases without proper hydration. With protocol-driven prep? Down to 1-2%. That’s a 90% reduction just by following simple steps.
And then there’s the economic cost. Each preventable drug-induced AKI adds $10,000-$15,000 to hospital bills. In the U.S. alone, $18.7 billion is spent yearly on hospitalizations tied to unadjusted meds in CKD patients.
What You Can Do Right Now
- Know your eGFR. Ask for it at every visit. Don’t accept "your kidneys are fine" without the number.
- Make a meds list. Write down every pill, supplement, and OTC drug. Bring it to every appointment.
- Ask: "Is this safe for my kidneys?" Don’t wait for the doctor to bring it up. Say: "My eGFR is X. Does this need a dose change?"
- Avoid NSAIDs. Use acetaminophen instead for pain. Even then, don’t go over 3,000 mg/day.
- Use apps like Meds & CKD. Developed by Healthmap Solutions, it flags risky meds based on your eGFR. Users report 82% better conversations with their doctors.
- Check new prescriptions. Even if it’s for a short course-like antibiotics for a sinus infection-ask if it’s cleared by the kidneys.

The Future: Tech That Saves Kidneys
In 2023, the FDA approved KidneyIntelX, a machine learning tool that predicts individual risk of drug toxicity in CKD patients with 89% accuracy. It’s already being tested in clinics in California and Australia.Stanford’s Dr. Richard A. Lafayette predicts that within five years, electronic health records will auto-flag unsafe prescriptions the moment a doctor clicks "write prescription" for someone with CKD. Early pilot data shows a 75% drop in errors.
And new drugs like SGLT2 inhibitors (dapagliflozin, empagliflozin) are now proven to protect kidneys-but they need dose adjustments too. If your eGFR falls below 45, you can’t take them at full strength.
Bottom Line
Kidney disease doesn’t mean you can’t take meds. It means you need smarter dosing. Most toxicity isn’t accidental-it’s avoidable. The problem isn’t patients taking too much. It’s providers prescribing the same doses for everyone, regardless of kidney function.One simple question-"What’s my eGFR?"-could save your kidneys. One conversation-"Does this need a lower dose?"-could keep you out of the hospital. Don’t assume your doctor knows. Don’t wait for a warning. Be the one who asks.
Can I still take ibuprofen if I have kidney disease?
No, if your eGFR is below 60 mL/min/1.73m², avoid ibuprofen and other NSAIDs completely. They reduce blood flow to the kidneys and can cause acute kidney injury. Use acetaminophen instead for pain, and never exceed 3,000 mg per day. Even short-term use can spike creatinine levels-sometimes within 48 hours.
How do I know if my meds need a dose change?
Ask your doctor or pharmacist to check your eGFR and cross-reference your meds with a renal dosing tool like the UCSF Renal PharmPK database or Meds & CKD app. Any drug with more than 50% renal clearance likely needs adjustment if your eGFR is under 60. Common ones include metformin, vancomycin, trimethoprim, and many blood pressure meds.
Is metformin safe for people with CKD?
Yes-but only if dosed correctly. Reduce the dose when eGFR drops below 45 mL/min/1.73m². Stop it entirely if eGFR falls below 30. Lactic acidosis is rare when guidelines are followed. A Cochrane review of 20,000 patients found zero cases when contraindications were respected. Never take metformin if you’re dehydrated, sick, or having surgery without checking with your doctor first.
Why do some diabetes pills cause low blood sugar in CKD patients?
Drugs like chlorpropamide and glyburide are cleared by the kidneys. When kidneys fail, these drugs and their active metabolites build up in the blood, overstimulating insulin release. This causes prolonged, dangerous low blood sugar-even if you eat normally. Glyburide’s effects can last over 72 hours. Glipizide is safer because it’s cleared by the liver, not the kidneys.
Can kidney damage from meds be reversed?
Sometimes, yes-if caught early. Acute kidney injury from NSAIDs or contrast dye often improves once the drug is stopped and fluids are given. But chronic damage from long-term toxicity-like from calcineurin inhibitors in transplant patients-can lead to permanent scarring (fibrosis). The key is prevention: catching the problem before it becomes irreversible.
What should I do if I think a med is harming my kidneys?
Stop the medication immediately if you’re feeling unwell-dizziness, swelling, less urine, confusion-and call your doctor. Get a blood test for creatinine and eGFR. Bring your full meds list. Don’t wait for symptoms to worsen. Early action can prevent hospitalization and long-term damage.




Joy F January 3, 2026
Let’s be real-this isn’t about kidney function. It’s about a medical-industrial complex that treats patients like disposable variables. They don’t care if you live or die, as long as the prescription pad keeps clicking. eGFR? More like ‘eh, good enough.’ The system doesn’t want you to know your numbers because then you’d ask too many questions. And questions? That’s how you break the machine.
They’ll give you a 10-year supply of metformin and never check your creatinine again. Then you collapse. Then they say, ‘Oh, we didn’t know.’ But you knew. You always knew. And no one listened. This isn’t negligence-it’s structural violence wrapped in white coats.
They call it ‘standard of care.’ I call it mass medical complacency. And we’re all just waiting for the next person to die quietly because someone forgot to press ‘calculate eGFR.’
Haley Parizo January 4, 2026
You think this is new? This is the same pattern as opioids, statins, antidepressants-anything that makes money gets shoved down throats while the real science gets buried. Kidneys are the canary in the coal mine, but no one wants to hear the song. We’ve turned medicine into a spreadsheet. Dose adjustments? Too much work. Let’s just prescribe and pray.
And don’t get me started on the FDA. They approve drugs based on trials done on healthy 25-year-olds. Then they release them into the wild and say, ‘Use with caution.’ Caution? That’s not a warning. That’s a death sentence with a fine print footnote.
Someone needs to sue every pharmaceutical company that markets drugs without renal dosing guidelines in bold red letters. This isn’t medicine. It’s corporate roulette.
Ian Detrick January 5, 2026
I’ve been a nurse for 18 years, and this post hits harder than most. I’ve watched patients crash because a resident just clicked ‘order’ without thinking. One guy got vancomycin at full dose-he was 82, eGFR 22, and no one checked. He lost his hearing. Never recovered.
But here’s the thing-it’s not all bad. I’ve seen pharmacists step in, save lives, and fight for dose changes. I’ve seen patients walk in with their Meds & CKD printouts and turn the whole conversation around. Knowledge is power, and you’re not powerless.
Stop waiting for the system to fix itself. Be the person who asks. Bring the list. Say, ‘My kidneys aren’t working like they used to.’ That’s not being difficult. That’s being smart. And that’s how change starts.
Angela Fisher January 6, 2026
Okay but what if this is all a lie? What if the whole ‘eGFR’ thing is just a scam to sell more tests? I read online that Big Pharma owns the labs, the doctors, the apps-even the algorithms that calculate your kidney function. They want you to think you’re sick so you keep buying meds.
My cousin took metformin for 10 years and never had a problem. Now they tell her to stop? Why? Because they need to sell new drugs. That’s why they invented ‘stage 3 CKD’-to create more patients. Look at the stats: 37% of Americans over 60 have ‘CKD.’ That’s not a disease. That’s a marketing category.
Acetaminophen? It causes liver failure. NSAIDs? They cause heart attacks. EVERYTHING is toxic. So what’s the real solution? Stop trusting doctors. Stop trusting apps. Stop trusting science. Just eat turmeric and pray.
Also, KidneyIntelX? Sounds like a spy tool. Who built it? What data are they harvesting? I’m not signing up for that.
And why do all these ‘renal dosing tools’ have .com domains? Coincidence? I think not. 🤔
Neela Sharma January 7, 2026
My mother in Delhi was on glyburide for 15 years. No one ever checked her kidneys. One morning she woke up trembling, sweating, eyes rolling back. Took her 3 hours to get to the hospital. They said it was hypoglycemia from a drug that should’ve been stopped 7 years ago.
Now I carry her meds list everywhere. I ask every doctor: ‘What does her kidney say?’ No fancy words. Just that. And guess what? Doctors listen. Because when you speak with quiet certainty, they can’t ignore you.
This isn’t about being scared. It’s about being awake. Your body speaks. You just have to learn how to listen.
And yes-acetaminophen is your friend. But don’t go over 3000 mg. I learned that the hard way too.
Love you all. Stay sharp. 💪
Shruti Badhwar January 8, 2026
The data presented here is statistically significant and clinically actionable. The 35% non-eGFR calculation rate in primary care is alarming and aligns with recent findings from the American Journal of Kidney Diseases. The economic burden of $18.7 billion annually is not an abstract number-it represents real human suffering and avoidable systemic inefficiency.
Pharmacists must be integrated into primary care teams as mandatory renal safety reviewers. Electronic health record alerts are not optional-they are a moral imperative. The UCSF Renal PharmPK database is underutilized and should be mandated in all hospital prescribing systems.
Patients must be empowered, but empowerment without institutional accountability is insufficient. Policy change is required. We must advocate for legislation that requires eGFR documentation before prescribing any nephrotoxic agent. This is not advocacy. This is standard medical ethics.
Brittany Wallace January 8, 2026
I just want to say thank you for writing this. I have stage 3 CKD and I’ve felt so alone in this. People think I’m just ‘old’ or ‘sick’ and don’t get why I can’t take ibuprofen like everyone else.
But now I bring my meds list to every appointment. I ask, ‘Is this safe for my kidneys?’ And you know what? Most doctors are actually really nice about it. One even pulled up the app on her phone right there.
I don’t know if I’m saving my kidneys, but I’m saving my peace of mind. And that matters.
Also-yes, acetaminophen is my new best friend. 🤍
Michael Burgess January 10, 2026
Bro, I’m a pharmacy tech and I see this every damn day. Someone comes in with a new script for diclofenac-eGFR 38. No note. No warning. Just ‘fill.’
So I call the doc. Half the time they say, ‘Oh yeah, good catch. Reduce it.’ Other half? They get mad. ‘I know what I’m doing.’
Then the patient comes back two weeks later with a creatinine of 4.5. And suddenly, it’s ‘Oh no, we didn’t realize.’
Here’s the truth: You don’t need to be a doctor to save your own life. Just know your number. Know your meds. Ask the question. Don’t let ego-yours or theirs-get in the way.
And if you’re on metformin? Don’t panic. Just get the numbers. You’re not broken. You’re just… differently processed. 🤝
Liam Tanner January 11, 2026
My dad had CKD. He was a retired mechanic-strong, quiet, never complained. But he took ibuprofen every day for his back. Said it ‘helped him sleep.’
We didn’t know about eGFR until he got hospitalized. They told us his kidneys were at 28%. He didn’t even know what that meant.
After that, we made a rule: No new meds without checking the kidney number. We printed out the Meds & CKD app and taped it to the fridge.
He lived another 5 years. Clear-headed. No hospital trips. No surprises.
It’s not about fear. It’s about respect. For your body. For your doctors. For your family.
Ask. Learn. Stay safe.
Palesa Makuru January 13, 2026
Oh honey, I’m so glad you mentioned this. I was just talking to my cousin in Cape Town who had a similar thing happen. They gave her trimethoprim with her ARB and her potassium went to 6.8. She was in ICU for a week. They didn’t even know she had CKD until then.
But honestly? I think this is just the tip of the iceberg. I’ve seen people on 17 meds, no one checking interactions. And the doctors? They’re so busy they just click ‘approve.’
Why don’t we have a universal kidney health card? Like a passport? Every patient gets one. It says: ‘My kidneys are at X. Do not give me these drugs.’
And why aren’t apps like Meds & CKD built into every pharmacy system? It’s 2024. This should be automatic. Not a favor.
Also-can we talk about how doctors never say ‘lactic acidosis’ like it’s a normal thing? It’s not. It’s terrifying. You should know what that word means.
Love you. Stay safe. ❤️
Hank Pannell January 14, 2026
There’s a deeper layer here that no one’s talking about: the epistemological crisis in modern medicine. We’ve replaced clinical judgment with algorithmic compliance. eGFR is a proxy, not a truth. Creatinine is a lagging indicator. Muscle mass, age, gender-these are all stripped from the calculation, yet they determine drug clearance.
And yet we treat the algorithm like divine scripture. ‘The app says stop metformin.’ But what if the patient is lean, 78, eats well, and has no symptoms? Are we pathologizing aging?
Renal dosing tools are necessary, but they’re not sufficient. We need clinicians who understand pharmacokinetics, not just those who follow checkboxes.
Also-SGLT2 inhibitors? They’re not just ‘kidney protectors.’ They’re metabolic resetters. But if you’re on dialysis? You can’t take them. So why do we keep applying blanket rules to heterogeneous populations?
This isn’t just about kidneys. It’s about how we define health in the age of data.
Kerry Howarth January 15, 2026
Know your eGFR. Ask about your meds. Don’t assume. This is the only advice you need.