COX-2 Inhibitor Cancer: Key Facts and Practical Insights
When talking about COX-2 inhibitors, a class of drugs that selectively block the cyclooxygenase‑2 enzyme. Also known as selective NSAIDs, they reduce the production of prostaglandins that drive pain and swelling. In the cancer arena, these agents have become a hot topic because they can modify the tumor micro‑environment.
One of the biggest drivers of tumor growth is chronic inflammation, a persistent immune response that fuels DNA damage and helps cancer cells evade death. COX-2 is often over‑expressed in many solid tumors, turning inflammation into a fuel source for cancer. By dialing down that enzyme, COX-2 inhibitor cancer strategies aim to cut the supply line that tumors rely on.
Among the many COX-2 inhibitors, celecoxib, the most widely studied drug in oncology often leads the conversation. Clinical trials have shown that celecoxib can slow the progression of colorectal, breast, and lung cancers when added to standard therapy. Its oral form and predictable dosing make it a practical option for patients looking to complement surgery or radiation.
Oncology, the medical specialty focused on cancer diagnosis and treatment has begun to treat COX-2 inhibition as a supportive measure rather than a stand‑alone cure. Doctors pair these drugs with chemotherapy, hoping the reduced inflammation will improve drug delivery to tumor cells and lessen side‑effects like nausea. Early evidence suggests that patients receiving both may experience longer progression‑free intervals.
Combining COX-2 inhibitors with traditional chemo also tackles a common hurdle: drug resistance. Cancer cells often adapt to harsh environments, but a less inflamed setting can make them more vulnerable to DNA‑damaging agents. This synergy has prompted several phase II studies where patients saw higher response rates than with chemo alone, especially in head‑and‑neck and ovarian cancers.
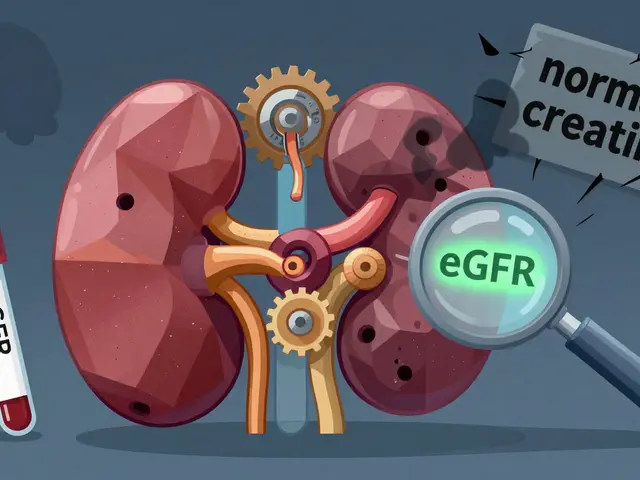
Safety remains a top concern. While COX-2 inhibitors spare the stomach lining, they can raise cardiovascular risk, especially in older adults with pre‑existing heart disease. Monitoring blood pressure, lipid profiles, and using the lowest effective dose helps balance benefit and risk. Patients should always discuss their full medical history with a clinician before adding any NSAID to a cancer regimen.
Choosing the right candidates involves looking for biomarkers like elevated COX‑2 expression in tumor tissue or high circulating prostaglandin levels. When these markers are present, the likelihood of a positive response improves. Personalized testing is becoming more accessible, allowing oncologists to tailor COX-2 inhibitor use to those who truly stand to gain.
The research pipeline is buzzing with next‑generation selective inhibitors that aim to keep the heart safe while hitting the tumor hard. Some of these newer molecules also target related pathways, such as the EP4 receptor, opening doors to combo therapies that could further suppress tumor growth. As trials progress, patients can expect more refined options that build on the groundwork laid by celecoxib.
Below you’ll find a curated list of articles that dive deeper into dosing tips, side‑effect management, real‑world case studies, and the latest trial results. Whether you’re a patient, caregiver, or health professional, these resources will give you actionable insights to navigate the evolving role of COX‑2 inhibitors in cancer care.
Celecoxib and Cancer Prevention: Latest Research Findings
Explore the latest research on celecoxib's role in cancer prevention, its effectiveness, safety concerns, and how it compares to other NSAIDs.