Breastfeeding and Asthma: What You Need to Know About Medications and Management
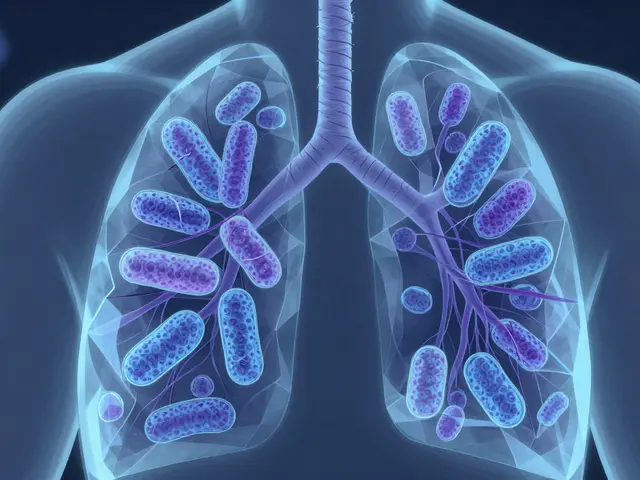
When you’re breastfeeding and managing asthma, a chronic condition that causes airway inflammation and breathing difficulties. Also known as reactive airway disease, it affects millions of new mothers who need relief without risking their baby’s health. The big question isn’t whether you can keep taking your meds—it’s which ones actually pass into breast milk, and in what amount. The good news? Most common asthma inhalers like albuterol and budesonide are considered safe. They’re designed to act locally in your lungs, so very little enters your bloodstream—and even less makes it into your milk.
But not all asthma treatments are created equal. Oral steroids like prednisone can raise concerns, especially with long-term use. Studies show that short courses are generally fine, but if you’re on daily doses, talk to your doctor about timing your doses right after a feeding. Meanwhile, lactation, the process of producing and releasing breast milk doesn’t just support your baby’s immune system—it can also influence how your body handles medication. Some moms notice their asthma worsens postpartum, not because of stress alone, but because hormones shift dramatically after birth. This isn’t just coincidence. Research from the American College of Allergy, Asthma & Immunology shows that up to 30% of women with asthma see changes in symptoms during pregnancy and the first few months after delivery.
And then there’s the baby. While asthma itself isn’t directly passed through breast milk, the risk of developing it can be influenced by early exposure. Breastfeeding lowers the chances of infant wheezing and respiratory infections, which are big triggers for future asthma. If your child has a family history of allergies or asthma, keeping your own symptoms under control is one of the best things you can do. Avoiding smoke, using air filters, and sticking to your inhaler plan aren’t just about you—they’re part of protecting your baby’s lung development.
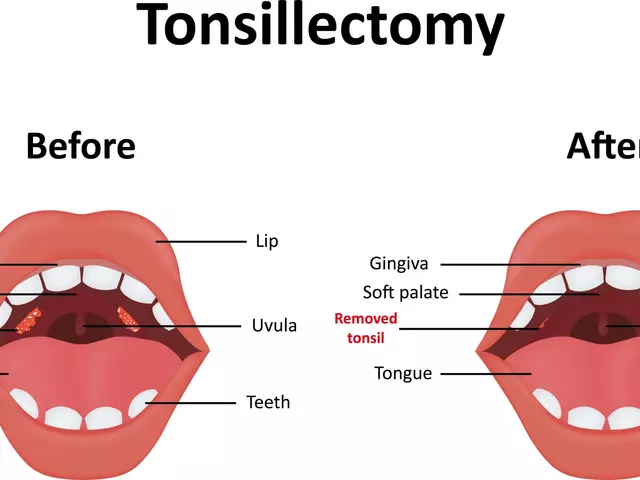
Some moms worry about antihistamines or decongestants. While non-drowsy antihistamines, medications like loratadine and cetirizine used for allergy relief are usually safe, oral decongestants like pseudoephedrine can reduce milk supply. That’s why many doctors recommend nasal sprays instead—they work locally and don’t hit your system hard. And if you’re using a steroid nasal spray like fluticasone? That’s also considered low-risk. It’s the same principle as inhalers: minimal absorption, minimal transfer.
You’re not alone in this. Many mothers balance asthma control with breastfeeding, and the science backs them up. The key is staying consistent—not skipping doses because you’re scared, and not switching to unproven remedies because you’re tired. If your symptoms change, if you feel worse, or if your baby seems unusually fussy or has trouble breathing, reach out. It’s not overreacting—it’s being smart.
Below, you’ll find real-world guides on asthma meds, postpartum health, and how to spot early signs of trouble in your baby. No guesswork. No fluff. Just what works, what doesn’t, and what your doctor might not have time to explain.
Asthma Medication Safety During Pregnancy and Breastfeeding: What You Need to Know
Learn the truth about asthma medication safety during pregnancy and breastfeeding. Discover which inhalers are safe, why stopping meds is riskier than using them, and how to manage asthma without fear.