Ear Infection Antibiotics: What You Need to Know
When dealing with ear infection antibiotics, medicines used to treat bacterial infections of the middle or outer ear. Also known as antibiotic ear drops, they aim to clear infection and reduce pain. Otitis media, the most common middle‑ear infection, especially in children is the primary condition these drugs target. The first‑line oral option is amoxicillin, a broad‑spectrum penicillin that works well for uncomplicated cases, while azithromycin, a macrolide often reserved for penicillin‑allergic patients provides a convenient once‑daily dosing schedule. A growing concern is antibiotic resistance, the ability of bacteria to survive standard treatments, which can limit the effectiveness of traditional choices. Understanding how these entities relate—ear infection antibiotics treat otitis media, require the right drug and dose, and are impacted by resistance—helps you make smarter treatment decisions.
Key Considerations When Choosing an Antibiotic
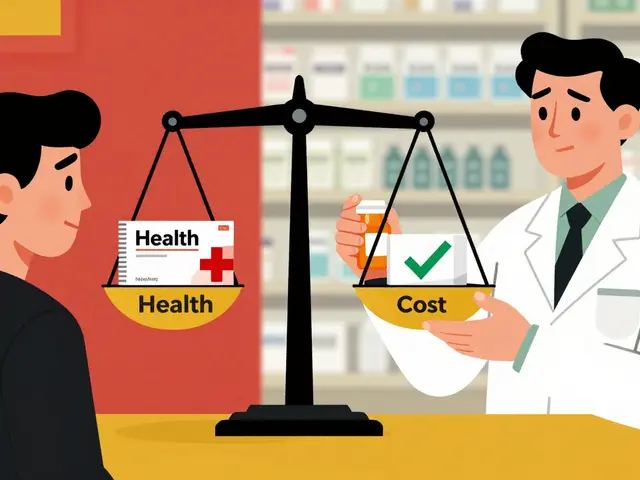
Choosing the right ear infection antibiotic starts with confirming a bacterial cause. A quick otoscopic exam can spot fluid behind the eardrum, indicating otitis media that’s likely bacterial. If symptoms have lasted less than 48 hours and are mild, many clinicians recommend a watch‑ful‑wait approach, especially for kids older than two, because viral infections resolve on their own. When antibiotics are needed, dosage matters: amoxicillin is typically given at 80‑90 mg/kg/day divided into two doses for children, ensuring blood levels stay above the minimum inhibitory concentration. For adults, a standard 875 mg dose twice daily works well. Azithromycin’s advantage is a shorter course—500 mg on day 1 followed by 250 mg daily for four more days—making adherence easier for travelers or busy parents. However, both drugs can cause side effects like diarrhea, rash, or, rarely, allergic reactions. If a patient reports a penicillin allergy, azithromycin or cephalosporins become the go‑to alternatives. Monitoring is crucial; if fever persists after 48‑72 hours of therapy, it may signal resistance, prompting a culture‑guided switch to a broader‑spectrum agent such as cefdinir or even a fluoroquinolone in severe cases.
Special populations need extra care. In infants younger than six months, the eustachian tube is shorter and more horizontal, increasing infection risk and often requiring a longer antibiotic course. For pregnant women, amoxicillin remains safe, but macrolides should be used only when necessary. Seniors may experience reduced kidney function, so dosing adjustments for drugs cleared renally, like amoxicillin, are essential. Beyond drugs, supportive care—warm compresses, adequate hydration, and pain relievers like acetaminophen—helps control discomfort while the antibiotic works. Finally, educating patients about completing the full course, even if symptoms improve, combats resistance and prevents recurrence. Below you’ll find a curated list of articles that dive deeper into each of these topics, from drug comparisons to dosing tables, giving you practical tools to manage ear infections confidently.
Cefprozil for Ear Infections: Dosage, Side Effects & Practical Tips
Learn how cefprozil treats ear infections, proper dosing, side‑effects, and practical tips to ensure a quick recovery.