Generic Substitution: What It Is, Why It Matters, and When to Watch for Side Effects
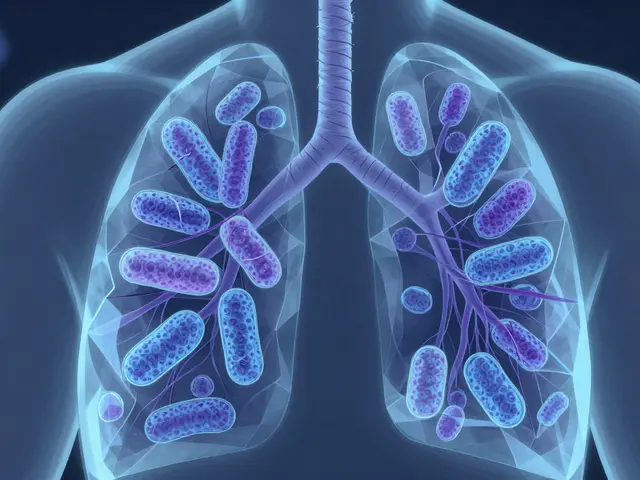
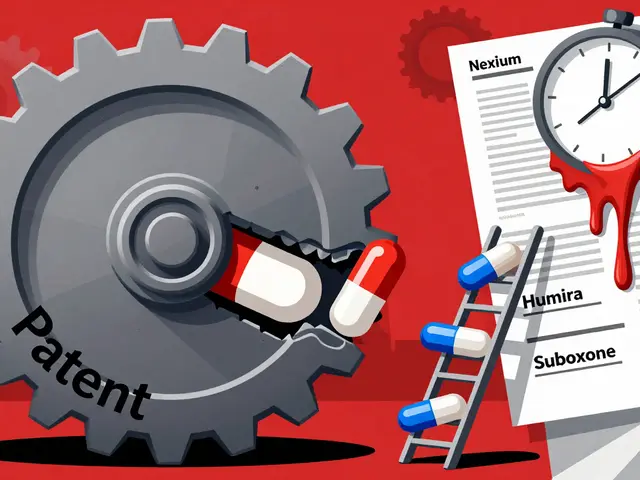
When your pharmacist hands you a pill with a different name than what your doctor wrote, that’s generic substitution, the practice of replacing a brand-name drug with a chemically identical generic version. Also known as therapeutic substitution, it’s one of the biggest cost-savers in modern healthcare—without sacrificing effectiveness for most people. The FDA requires these generics to deliver the same active ingredient, in the same strength, and with the same effect as the original. That’s not marketing—it’s science. But here’s the thing: even if two pills have the same active ingredient, how your body absorbs them can vary slightly. That’s where bioequivalence, the measure of how similarly a generic drug performs compared to the brand comes in. For most drugs, those tiny differences don’t matter. But for drugs with a narrow therapeutic index—like blood thinners, thyroid meds, or seizure drugs—even a small change can trigger side effects or make the treatment less effective.
That’s why switching to generics, the process of changing from a brand-name drug to its generic equivalent isn’t just a pharmacy transaction. It’s a health decision. Many people never notice a difference. Others report new side effects—nausea, dizziness, or a return of symptoms they thought were under control. This isn’t always about the drug itself. Sometimes it’s about the fillers, the coating, or even how the pill breaks down in your stomach. And while generic drug safety, the assurance that generic medications meet the same quality standards as brand-name drugs is backed by strict testing, real-world use doesn’t always match lab results. That’s why knowing the warning signs matters. If you feel worse after a switch, don’t assume it’s all in your head. Document it. Talk to your doctor. It might be nothing. Or it might be your body reacting to a change in how the drug is delivered.
What you’ll find below is a collection of real, practical guides that cut through the noise. We cover how to spot when a generic switch might be risky, why some generics fail silently, how regulators test them, and what to do if your blood pressure spikes or your asthma gets worse after the switch. You’ll also learn how pharmacy inventory systems prioritize generics, why some manufacturers are going out of business, and how even something as simple as pill shape can affect how you take your medicine. This isn’t theory. It’s what people are actually experiencing—and what you need to know before your next refill.
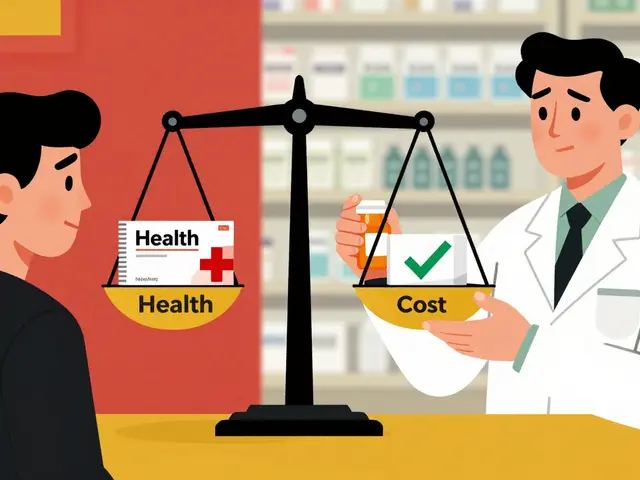
Medication Therapy Management: How Pharmacists Optimize Generic Drug Use for Better Outcomes
Pharmacists play a critical role in Medication Therapy Management by optimizing generic drug use to improve adherence, reduce costs, and prevent adverse events. Learn how MTM works, why generics matter, and what patients can do to access these services.
Pharmacist Responsibilities When Dispensing Generics: Legal Obligations Explained
Pharmacists must follow strict legal rules when dispensing generic medications. These include state-specific consent laws, restricted drug lists, and documentation requirements. Failure to comply can lead to disciplinary action and patient harm.