Generic Drug Market: What You Need to Know About Savings, Safety, and Choices
When you hear generic drug market, the global system of non-brand medications sold after patents expire. Also known as off-patent drugs, it's the backbone of affordable healthcare for millions. It’s not a shadow economy—it’s a regulated, science-backed system that delivers the exact same active ingredients as brand-name pills, but without the marketing costs. The generic drug market isn’t just about saving money—it’s about making sure people can actually afford to stay healthy.
Every generic drug must pass strict tests to prove it works just like the brand version. This is called bioequivalence, the scientific proof that a generic drug delivers the same amount of medicine into your bloodstream at the same rate as the brand. It’s not guesswork. Regulators like the FDA and EMA require this for every single generic. That’s why a $5 generic pill for high blood pressure has the same effect as its $100 brand-name cousin. And it’s why switching doesn’t mean settling—it means smart choices.
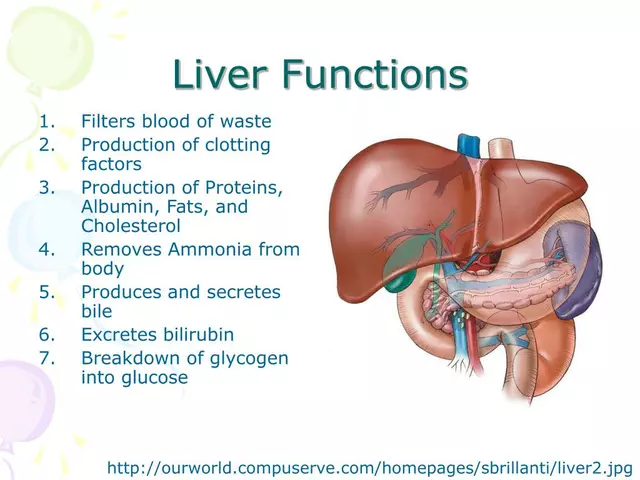
Some people worry generics aren’t as safe, but that’s a myth. The same factories often make both brand and generic versions. The only differences? The color, shape, or inactive fillers—things that don’t affect how the medicine works. What matters is the active ingredient, and that’s locked in by law. Even complex forms like inhalers, patches, and injections must match the original in how they deliver the drug to your body. That’s why brand name drugs, originally developed and marketed under a proprietary name. still dominate headlines, while generics quietly keep the system running.
And the numbers don’t lie. Generics make up over 90% of all prescriptions filled in the U.S.—but cost only 15% of what brands do. That’s billions saved every year by families, insurers, and public health programs. The drug pricing, the cost structure of medications influenced by patents, competition, and regulation. system works because generics force brands to drop prices or lose market share. It’s capitalism at its most practical: competition lowers costs without lowering quality.
Still, not every switch is seamless. Some drugs have a narrow therapeutic window—tiny changes in dosage can cause big effects. That’s why you might notice side effects after switching, like nausea or dizziness. It’s rare, but real. That’s why knowing the warning signs matters. And why some doctors still hesitate to switch patients on certain meds, even when the science says it’s safe.
Behind the scenes, the generic drug market is changing fast. New combo pills—like a single tablet with three blood pressure drugs—are hitting shelves. These "super generics" make it easier to take multiple meds, which means fewer missed doses and better outcomes. Meanwhile, stability testing keeps track of how these drugs break down over time. Packaging, humidity, heat—all of it gets tested to make sure your pill still works when you open it six months later.
What you’ll find here isn’t marketing fluff. It’s real talk from people who’ve switched, doctors who’ve seen the results, and scientists who’ve tested the data. You’ll learn when generics are perfect, when to watch out, and how to talk to your pharmacist about your options. No jargon. No hype. Just what you need to know to make the right call for your health—and your wallet.
How Multiple Generic Drug Manufacturers Lower Prices
Multiple generic manufacturers drive down drug prices through competition, saving patients billions. Learn how the number of makers affects cost, why some drugs stay expensive, and how to save on prescriptions.
Generic Manufacturer Profitability: Business Models and Sustainability
Generic drugs save billions in healthcare costs, but most manufacturers are losing money. Discover why simple generics are collapsing, how complex drugs and contract manufacturing are reshaping the industry, and what it means for medicine access.