Senior Medication Dosing: What Works, What Doesn't, and How to Stay Safe
When it comes to senior medication dosing, the way drugs are adjusted for older adults based on changes in metabolism, kidney function, and body composition. Also known as geriatric pharmacology, it’s not just about taking less—it’s about taking differently. Your body changes after 65. Your kidneys don’t filter as fast. Your liver slows down. Fat replaces muscle. That means a pill that was perfectly safe at 50 can become dangerous at 75—even if the dose hasn’t changed.
This is why polypharmacy, the use of multiple medications at once, often by older adults. Also known as multiple drug therapy, it’s one of the biggest risks in senior care. More than 40% of seniors take five or more prescriptions daily. Each one adds risk. A blood thinner like warfarin might be fine on its own, but add it to an NSAID for joint pain, and bleeding risk spikes. Add a sleep aid, and dizziness turns falls into fractures. It’s not the drugs themselves—it’s the combo, the dose, and the body’s ability to handle them.
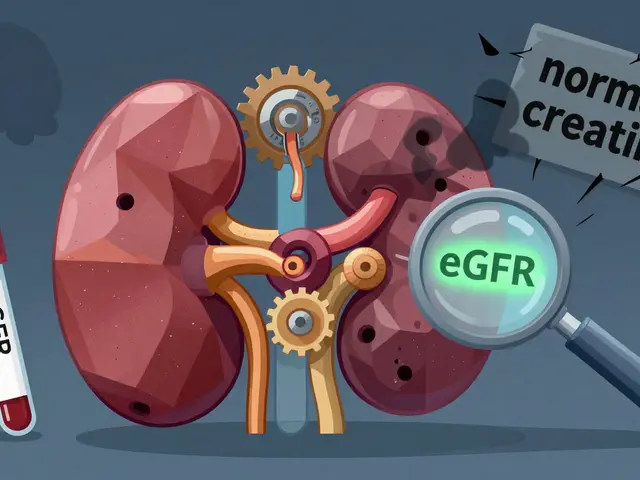
kidney function in seniors, how the kidneys’ ability to clear drugs declines with age, often without symptoms. Also known as reduced glomerular filtration rate, it’s a silent factor in most bad reactions. Doctors often still use the same dosing rules for everyone, but your kidneys aren’t working like they did at 30. A standard dose of a diuretic or antibiotic might build up to toxic levels. That’s why creatinine tests and eGFR numbers matter more than age alone. And yet, too many prescriptions ignore this.
Side effects in seniors don’t always look like nausea or rash. Sometimes it’s confusion, falling, fatigue, or loss of appetite. These aren’t "just getting older"—they’re warning signs. A study in the Journal of the American Geriatrics Society found that nearly 25% of hospital admissions for seniors are tied to medication problems. Most of them were preventable.
What’s missing from most conversations is the balance. Stopping a drug isn’t always safer than keeping it. A blood pressure pill might cause dizziness, but stopping it raises stroke risk. An antidepressant might make you sleepy, but untreated depression speeds up cognitive decline. The goal isn’t fewer pills—it’s the right pills, at the right dose, for your body right now.
That’s where the posts below come in. You’ll find real-world breakdowns of how anticoagulants behave in older bodies, why NSAIDs are riskier after 70, how generic drugs stack up for seniors, and what to watch for after switching meds. We cover dosing pitfalls with blood thinners, the hidden dangers of OTC sleep aids, and how to talk to your pharmacist about adjusting doses without sounding like you’re questioning your doctor. This isn’t theory. These are the mistakes that land people in the ER—and how to avoid them.
Medication Dosage Adjustments for Aging Bodies and Organs: What Seniors and Caregivers Need to Know
Aging changes how your body handles medications. Learn why seniors need lower doses, which drugs are risky, and how to prevent dangerous side effects with proven strategies from geriatric experts.